Alveolar Hemorrhage in Lupus Needs Prompt Evaluation Save
Acute diffuse lung infiltration in patients with systemic lupus erythematosus (SLE) requires prompt evaluation for diffuse alveolar hemorrhage (DAH) when patients have low levels of hemoglobin and complement compound C4 and symptoms of hypoxia. The development of DAH was significantly associated with the presence of these features, South Korean researchers have found. (Citation Source http://buff.ly/2uSPVK7)
In their retrospective series of 47 SLE patients with acute diffuse lung infiltration, about half satisfied criteria for DAH, and although mortality was no different between patients with or without DAH (29.2% versus 21.7%), more than 80% of the patients with DAH who died did so within 3 weeks.
Because of this risk of early death, "we consider that early detection of diffuse lung infiltration and early suspicion of DAH will be key factors in improving the prognosis of DAH in SLE patients," wrote Dam Kim, MD, PhD, from Hanyang University Hospital for Rheumatic Diseases, Seoul, South Korea, and colleagues.
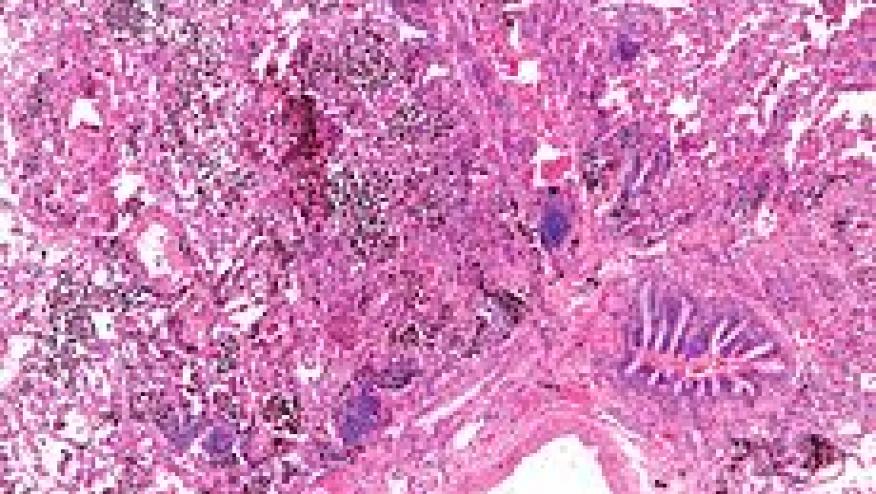
Acute diffuse alveolar infiltration is a rare manifestation of SLE. Among its causes are acute pneumonitis and DAH, which are life threatening. DAH is characterized by acute diffuse lung infiltration; clinical symptoms are non-specific.
As they reported in Seminars in Arthritis and Rheumatism, the investigators selected 47 patients with acute diffuse lung infiltration from a total of 815 SLE patients who underwent thoracic computed tomography (CT) scans at a single academic hospital.
The criteria to satisfy a diagnosis of DAH were the presence of acute diffuse lung infiltrationon thoracic CT scans, a reduction in hemoglobin (Hb) level ≥41.5 g/dL compared with the level before hospitalization or an Hb level of ≤10.0 g/dL at the time of the thoracic CT scan and one or more pulmonary symptoms or signs (i.e., hemoptysis, dyspnea, cough, sputum, hypoxia). Of the 47 SLE patients with acute lung infiltration, 24 (51%) satisfied these criteria and constituted the DAH group and 23 (49%) did not. Hb (8.2 7 versus 10.0 g/dl, P<0.01) and C3 (41.0 versus 63.4, P<0.04) levels were significantly lower in the DAH group compared with the non-DAH group. The SLEDAI-2K score (11.5 versus 10.1, P< 0.52), C4 level (10.7 versus 17.0, P=0.11) and CH50 level (15.6 versus 26.6, P=0.19) were not significantly different between the two groups.
The DAH group had lower Hb (OR 1.75, 95% CI 1.19-2.58, P<0.01), lower C3 (OR 1.03, 95% CI 0.00-1.05, P=0.02), and lower C4 (OR 1.07, 95% CI 1.00-1.14, P=0.049) levels at the time of diagnosis. Initial symptoms such as the presence of hemoptysis, dyspnea, hypoxia and absence of fever showed trends toward an association with DAH that were not statistically significant.
In an adjusted analysis, decreased levels of Hb (OR 3.46, 95% CI 1.38-8.6, P<0.01) and C4 (OR 1.21, 95% CI CI: 1.03-1.42, P=0.02) were independent risk factors for DAH. Among the initial symptoms, the presence of hypoxia (OR 23.09, 95% CI 1.47-365.34, P=0.03) was also independently associated with DAH.
Seven patients (29.2%) in the DAH group died compared with five (21.7%) in non-DAH group (P=0.42). "Although the mean duration from DAH diagnosis to death was 53.7 days, more than half the patients died within 3 weeks," wrote Kim and co-investigators. "Of the seven deceased DAH patients, six died within 3 weeks of the onset of DAH, while one of the five deceased non-DAH patients also died within 3 weeks of the onset of acute diffuse lung infiltration (P=0.056)."
In multivariable analysis, a severe condition requiring mechanical ventilation (OR 64.61, 95% CI 1.98-2112.02, P=0.02) was associated with an increased mortality, but DAH was not.
Among patients with SLE-DAH, lupus nephritis was the most important clinical feature associated with death (100% versus 35.3%, P<0.01). Patients with SLE-DAH who died had received more intensive treatments involving plasmapheresis (71.4% versus 17.6%, P=0.02), intravenous immune globulin (85.7% versus 35.3%, P=0.07), transfusion (100% versus 47.1%, P=0.02) and mechanical ventilation (71.4% versus 0%, P<0.01) compared with the survivors. The authors speculated that receiving intensive treatment "is probably not a risk factor for mortality but an indicator of the severity of DAH."
Among the limitations was the inclusion of only 24 DAH patients due to the low incidence of DAH, leaving inadequate statistical power for some comparisons.
"A study of even more patients, or a meta-analysis, should provide conclusive findings regarding the risk factors for mortality," the authors wrote.







If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.