High GPA Hospital Readmission Rates Save
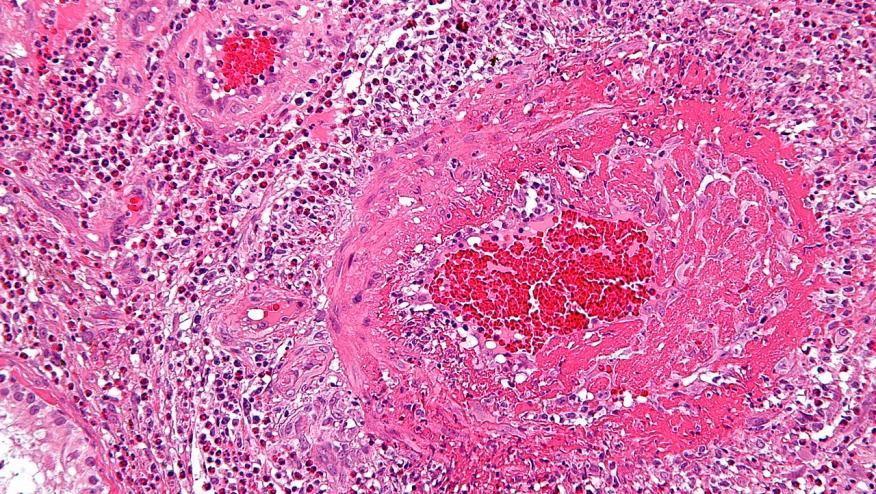
A national database reveals that patients with granulomatosis with polyangiitis (GPA) have 22.3% risk of hospital readmissions within 30 days of discharge.
From a total of 9749 hospital admissions with GPA, there were 2173 readmissions within 30 days of discharge.
The top 5 reasons for readmissions were:
- GPA
- Sepsis
- Pneumonia
- Acute respiratory failure
- Acute kidney injury
GPA requiring readmissions were associated with higher length of stays and predictors were were younger age (OR 0.99; p = 0.013), no private insurance (OR, 0.50; p < 0.001), more comorbidity (OR, 1.12; p = 0.039), congestive heart failure (OR, 1.71; p = 0.001), acute kidney injury (OR, 1.39; p = 0.005), and discharge to home health care (OR, 1.29; p = 0.039).
A signficant risk of readmission faces patients with GPA, especially those with younger age, public insurance, higher comorbidity burden, cardiac and renal complications.







If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.