High Mortality with ANCA Associated Vasculitis Save
Mortality remains high in patients with the types of vasculitis that are associated with the presence of antineutrophil cytoplasmic antibodies (ANCA), a meta-analysis in Annals of the Rheumatic Diseases determined.
Compared with the general population, patients with ANCA-associated vasculitis had a 2.7-fold increased mortality, with a meta-standardized mortality ratio (SMR) of 2.71 (95% CI 2.26-3.24), reported J. Antonio Avina-Zubieta, MD, PhD, of the University of British Columbia in Vancouver, and colleagues.
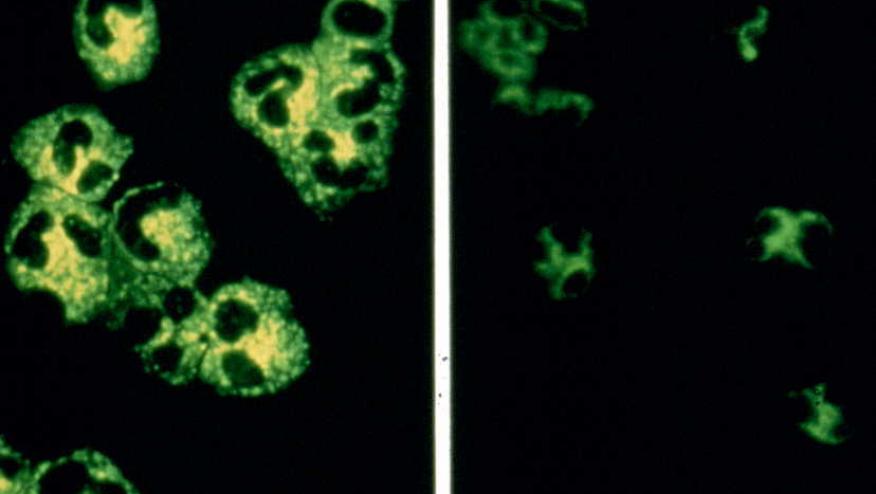
The systemic vasculitides are a group of disorders characterized by inflammation of the walls of blood vessels, with ANCA playing an important pathologic role in the small vessel vasculitides. These include granulomatosis with polyangiitis (GPA), microscopic polyangiitis (MPA), and eosinophilic granulomatosis with polyangiitis (EGPA).
Prior to the 1960s, when treatment with glucocorticoids and cyclophosphamide was introduced, the mean survival time following a diagnosis of GPA was only 5 months. Today, 1-year survival for patients with GPA has been estimated to be 81% to 95%, while 5-year and 10-year survival rates range from 73% to 83% and 55% to 75%, respectively.
For MPA, survival rates at 1, 5, and 10 years have been estimated at 80%, 45% to 85%, and 74%, while 5-year survival for EGPA has been reported at 89% to 97%.
Despite these improvements in survival, however, some studies have suggested that the risks of death remain higher for these groups of patients, while other reports found no differences.
Avina-Zubieta's group explained that their research was prompted by the fact that previous studies were limited by small numbers of patients and different types of cohorts; the team, therefore, undertook a literature search for relevant publications during the past 4 decades.
Of the 570 abstracts identified, 10 met the inclusion criteria and were included in the meta-analysis. These included 14 distinct cohorts and 3,338 patients who had been enrolled from 1966 to 2009. A total of 2,619 patients had been diagnosed with GPA, 501 with MPA, 185 with EGPA, and an additional 33 were classified as having renal limited vasculitis.
Three of the studies were population-based, while seven were hospital- or clinic-based. In four studies, only patients with GPA were included.
There were 1,091 observed deaths through 2015.
The mortality risk was similar to the overall standardized mortality ratio when the analysis was restricted to patients with GPA (meta-SMR 2.63, 95% CI 2.02-3.43), the team found.
In five of the studies, risks were evaluated separately according to gender. No difference was seen, with a meta-SMR of 3.36 (95% CI 2.10-5.38) for women and 3.11 (95% CI 2.21-4.36) for men.
That observation differed from what was seen in an earlier study from a German vasculitis center, in which young men with GCA had a substantially higher risk of death than young women with the disease (SMR 8.87, 95% CI 4.05-16.8). This was attributed to more frequent kidney involvement in the men.
Significant heterogeneity was found among the different cohorts (I2 = 84.4%, 95% CI 72.6-96.3). Subgroup analyses identified several differences that might have affected the results, such as higher meta-SMRs being seen in multicenter studies, in non-inception cohorts, in population-based studies, and in groups enrolled before 2000. Only the comparison of risk between multicenter and single-center cohorts was statistically significant (meta-SMR 3.27, 95% CI 2.73-3.91 versus 1.89, 95% CI 1.17-3.07, P=0.05).
The authors noted that it was "of interest" that cohorts with the midpoint of enrollment in earlier years had higher mortality risks, although the difference again was not statistically significant:
- 1980-1993, SMR 3.43 (95% CI 2.79-4.21)
- 1994-1999, SMR 2.82 (95% CI 2.14-3.72)
- 2000-2005, SMR 1.92 (95% CI 1.12-3.29)
And, the authors wrote, despite the lack of statistical significance, "we hypothesize that this observation may have resulted from therapeutic improvements, earlier diagnosis with increased availability of ANCA testing and increased physician awareness, as well as improved overall patient care in terms of cardiovascular risk modification, drug toxicity prevention strategies, and cancer surveillance."
Limitations of the study included differences among the cohorts, including varying degrees of renal involvement.
"There is a need for longitudinal studies in contemporary cohorts to evaluate mortality benefits of modern therapies," Avina-Zubieta and colleagues concluded.







If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.