Nailfold Capillary Density Predicts Dermatomyositis Lung Involvement Save
In patients with juvenile dermatomyositis (DM), an association was seen between low nailfold capillary density and pulmonary involvement, European researchers reported.
Among patients whose nailfold capillary density was less than 6/mm, forced vital capacity (FVC) was 89.7% predicted compared with 98.5% predicted for those with normal capillary density (P=0.008), according to Helga Sanner, MD, PhD, of Oslo University Hospital in Norway, and colleagues.
In addition, total lung capacity (TLC) was 87.8% predicted in those with low capillary density compared with 94.5% (P=0.020), while low diffusion capacity for carbon monoxide (DLCO) was found in 71% compared with 38% of those with normal density (P=0.014), the researchers reported online in Arthritis Care & Research.
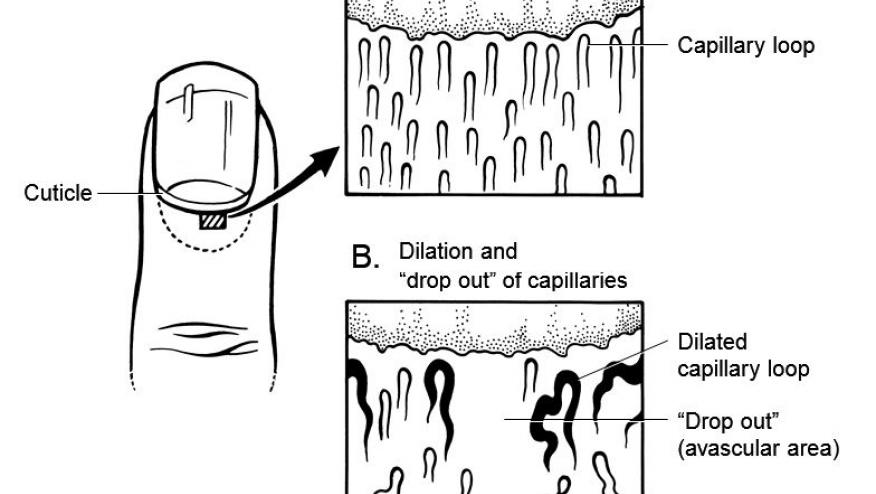
"Nailfold capillaroscopy is a simple, noninvasive technique to evaluate the microvascular architecture," they wrote.
Studies of adult patients with systemic sclerosis have found associations between abnormalities of the microvasculature detected on nailfold capillaroscopy and pulmonary or cardiac involvement, but no studies thus far have considered the possibility of these associations in pediatric rheumatic diseases such as juvenile DM.
Sanner's group has established a long-term cohort of 58 Norwegian patients diagnosed with juvenile DM from 1970 to 2006 who have been closely followed with nailfold capillaroscopy and pulmonary/cardiac assessments. In previous reports, the team noted that their patients had smaller lung volumes and lower diffusion capacity than healthy controls, along with decreased systolic and diastolic function.
Almost two-thirds of the cohort were female, and mean age at the time of the current analysis was 25.4; disease duration was 17 years.
Pulmonary function was assessed with spirometry, and high-resolution computed tomography (CT) was used to detect interstitial lung disease or other abnormalities such as bronchiectasis. Cardiac assessment included echocardiography and electrocardiography.
Nailfold capillaroscopy found that 36% of patients had low capillary density and identified a neovascular pattern in 41%.
Along with decreased capacity on pulmonary function testing, 30% of patients with low capillary density showed evidence of airway disease on high-resolution CT compared with only 8% of those with normal density (P=0.034).
After adjustment for the association between capillary density and age and disease duration, an association between TLC % predicted and capillary density persisted (β = 0.295, P=0.018), although the association with FVC % predicted did not.
On cardiac measures, no significant differences were observed between patients with low and normal nailfold capillary density, including ECG findings, heart rate variability, and systolic or diastolic function.
"Our key finding is the relationship between low nailfold capillary density and smaller lung volumes (FVC and TLC) and reduced gas diffusion (low DLCO) in juvenile DM," the authors wrote.
They noted that their study found decreased lung volumes and a higher incidence of airways disease detected on high-resolution CT, but a sizeable number of patients whose capillary density was normal also had pulmonary abnormalities.
"Thus, even if microvascular involvement seems to be relevant in the development of pulmonary manifestations, other factors are likely to contribute to the process in juvenile DM."
Subclinical cardiac involvement has been detected in up to one-quarter of patients with juvenile DM, but the study does not support the hypothesis that vasculopathy is the underlying mechanism, the researchers said, noting, though, that the study was too small to provide definitive conclusions on this.
"Further and preferably larger studies are needed to identify nailfold capillary density as a potential biomarker for organ involvement," the researchers concluded.







If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.