New EULAR Guidelines for Ultrasound Use Save
In the current issue of ARD, the European League Against Rheumatism (EULAR) has revised and updated its 2001 guideline for musculoskeletal (MS) ultrasound (US) in rheumatology; this time incorporating new advances, technological developments and use indications in rheumatology. EULAR has provided this as an educational tool and standard reference for MSUS practice and research in rheumatology.
US is here to stay. A recent survey of rheumatology fellowship programs showed that MS US is currently being taught in 94% of programs, with 41% having a formal MSUS curriculum.
These new guidelines are based on: (1) a systematic literature review of MS US evaluable structures; (2) a Delphi survey among rheumatologist and radiologist experts in MS US to select MS and non-MS anatomic structures and abnormalities evaluable by US that are relevant to rheumatology; and (3) a nominal group technique to achieve consensus on the US scanning procedures and to produce an electronic illustrated manual and App of these procedures.
Task force consensus-based recommendations for comprehensive and standardised procedures for MSUS imaging in rheumatology include:
Recommended Procedures
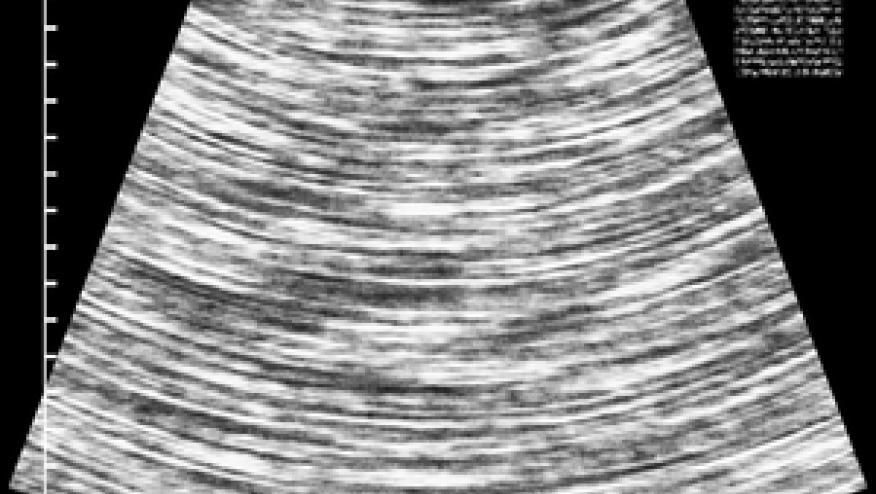
- MSUS includes two principal modes: B-mode (or grey scale) that provides us with morphological information of the anatomic structures and Doppler mode (colour Doppler or power Doppler) that allows us to evaluate blood flow.
- MSUS should be performed with high-resolution linear transducers (ie, probes) with frequencies between 6 and 14 MHz for deep/intermediate areas to ≥15 MHz for superficial areas.
- Tissue harmonic imaging, spatial compound imaging, extended field of view (panoramic) and virtual convex imaging are some of the software capabilities that may be useful in MSUS.
- When scanning a joint, the probe should be oriented as perpendicular or parallel to the bony cortical surface (bony acoustic landmark) so that the cortical margin appears bright, sharp and hyperechoic.
- A dynamic scanning technique by means of slight movements of translation (side-to-side, back-to-front), angulation and rotation of the probe should be carried out in order to allow the best visualisation of the structure(s) of interest.
- MS structures should be evaluated as they move smoothly either actively or passively.
- To avoid anisotropy (ie, hypoechoic/anechoic appearance of a normally hyperechoic structure that mainly affects tendons) and the common pitfalls that accompany it, the probe should be continuously adjusted to maintain the beam perpendicular to the tendon fibres especially in insertional regions.
- When the long axis of the structure of interest corresponds to the cranial-caudal orientation of the anatomic position, the most proximal aspect of the structure is usually placed on the left-hand side of the screen. However, other options are acceptable as long as the movement of the image on the screen is kept parallel to the direction of the probe on the patient. Our preference for short axis is to align the structure of interest on the screen as if the observer is looking at the patient.
- Probe compression can be helpful in distinguishing a compressible liquid collection from a non-compressible solid. Little or no compression is important when performing Doppler examination to avoid cessation of flow in small vessels.
- A generous amount of gel should be used for superficial structures especially when little or no pressure is indicated.
- The machine setting for B-mode and Doppler mode should be properly adjusted to optimise the US image acquisition process.
Recommended Structures
- 9 anatomic areas/organs/systems (i.e., shoulder, elbow, wrist and hand, hip, knee, ankle and foot, peripheral nerves, salivary glands and large vessels) were selected for MSUS.
EULAR US Scanning App







If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.