SAPHO Syndrome Revisted Save
SAPHO is an acronym that describes a constellation of findings (synovitis, acne, pustulosis, hyperostosis, and osteitis) that defines this rare syndrome.
While its true incidence is unknown and the condition may often be misdiagnosed or underrecognized, the SAPHO syndrome falls within a variety of disorders manifesting reactive osteitis, arthritis, and chronic cutaneous pustular lesions.
Although the etiology of the SAPHO syndrome is unknown, it is considered to be reactive inflammatory disorder linked to its hallmark pustulosis, followed by subsequent osteitis, and other similarities with the the spondyloarthropathies.
This rare disorder affects males and females equally and while most reports come from Japan, many cases have been seen in Caucasians in Scandinavia, France and the United States.
Skeletal disease develops after established pustulosis (i.e., palmoplantar pustulosis, acne conglobata, acne fulminans, hidradenitis suppurativa, pustular psoriasis).
Painful, nodular swelling of skeletal lesions characterized by development of early erosive and late hyperostotic changes in the joints of the anterior chest wall or axial skeleton. The anterior chest wall and axial skeleton are preferentially targeted. Affected amphiarthroses (saddle joints) of the anterior chest wall include the sternoclavicular, manubriosternal, and sternocostal joints. Peripheral involvement of the hands and feet is uncommon.
Spondylodiscitis and enthesitis are sometimes seen. Chronic relapsing pustular lesions may affect palms or soles (palmoplantar pustulosis), intertriginous areas (hidradenitis), or face, trunk, and extremities (acne).
There are no diagnostic tests, but mild to moderate elevation of the acute-phase reactants and increased leukocyte counts are common and HLA-B27 is positive in 30% of patients.
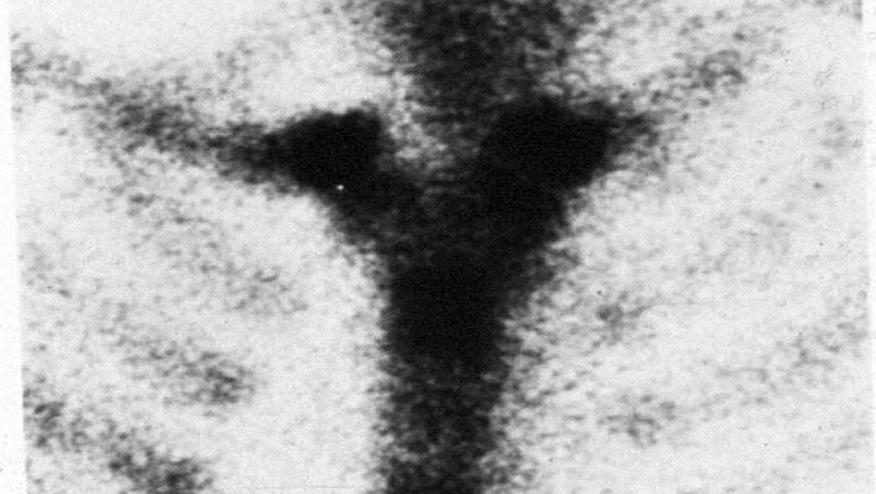
Early in the disease, radiographs show erosive changes in the anterior chest wall joints, sometimes accompanied by subchondral sclerosis and periostitis. With chronicity, subchondral sclerosis and hyperostosis ensue. Bony ankylosis is uncommon. Spondylodiscitis is the most common axial finding and is suggested by erosions of the vertebral plates with reactive vertebral sclerosis. Sacroiliitis is seen in as many as one-third of patients. Bone scans reveal increased uptake in affected skeletal areas (see image).
Topical and systemic therapies are directed at the underlying pustular disorder. The musculoskeletal manifestations are often difficult to treat, although most individuals exhibit some response to systemic antibiotics, NSAIDs, and oral or intraarticular corticosteroids. DMARDs and immunosuppressive drugs in SAPHO have yielded variable results.
While there are no clinical trials, numerous reports suggest that TNF inhibitors (TNFi) may be effective in those with unresponsive or refractory SAPHO. Also promising has been the use of anakinra, ustekinumab and the potential benefit to IL-17 blockade (e.g., secukinumab) in difficult-to-treat SAPHO cases.
(content exerpted with permission from RheumaKnowledgy.com. Citation source: http://buff.ly/2anJN2t)







If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.