What is Colchicine Worth? (6.23.2023)
Dr. Jack Cush reviews the news and reports from the past week on RheumNow.com. This week a new colchicine FDA approval, rising rate of IgG4 related disease and what's the safest biologic?

Dr. Jack Cush reviews the news and reports from the past week on RheumNow.com. This week a new colchicine FDA approval, rising rate of IgG4 related disease and what's the safest biologic?
Dr. Jack Cush reviews the news and journal reports from this past week on RheumNow.com. This week we delve into some odd associations, repeat drug warnings and the consequences of antirheumatic therapies.
This week on the Podcast Dr. Jack Cush reviews the news and journal articles, including the risks of dying, developing RA or autoimmune disease!
Does King Charles have Sausage Digits (dactylitis) or OA? https://t.co/mRis21OWKH
Opportunistic and chronic infections may be rare and are often difficult to diagnose, especially in patients with autoimmune inflammatory rheumatic diseases (AIIRD), that may be immunocompromised.
Having their clinics shut down and patients staying away during the COVID-19 pandemic was bad enough for physicians' finances, but now a new study finds that, at least for rheumatologists, payments from industry dried up as well.
This week on the podcast, Dr. Jack Cush recalls what life was like early on during COVID, from March to June of 2020. During this time, his close friend, Larry, contracted COVID-19 and was hospitalized, intubated and put on mechanical ventilation for nearly 2 months.
Dr. Jack Cush reviews the best of 2022 in Rheumatology - highlights on new drug indications, breakthrough lupus therapies, new biosimilars and the multivitamin letdown.
Editor's note: this blog originally published on January 22, 2022, and is being shared again as a Best of 2022. Enjoy!
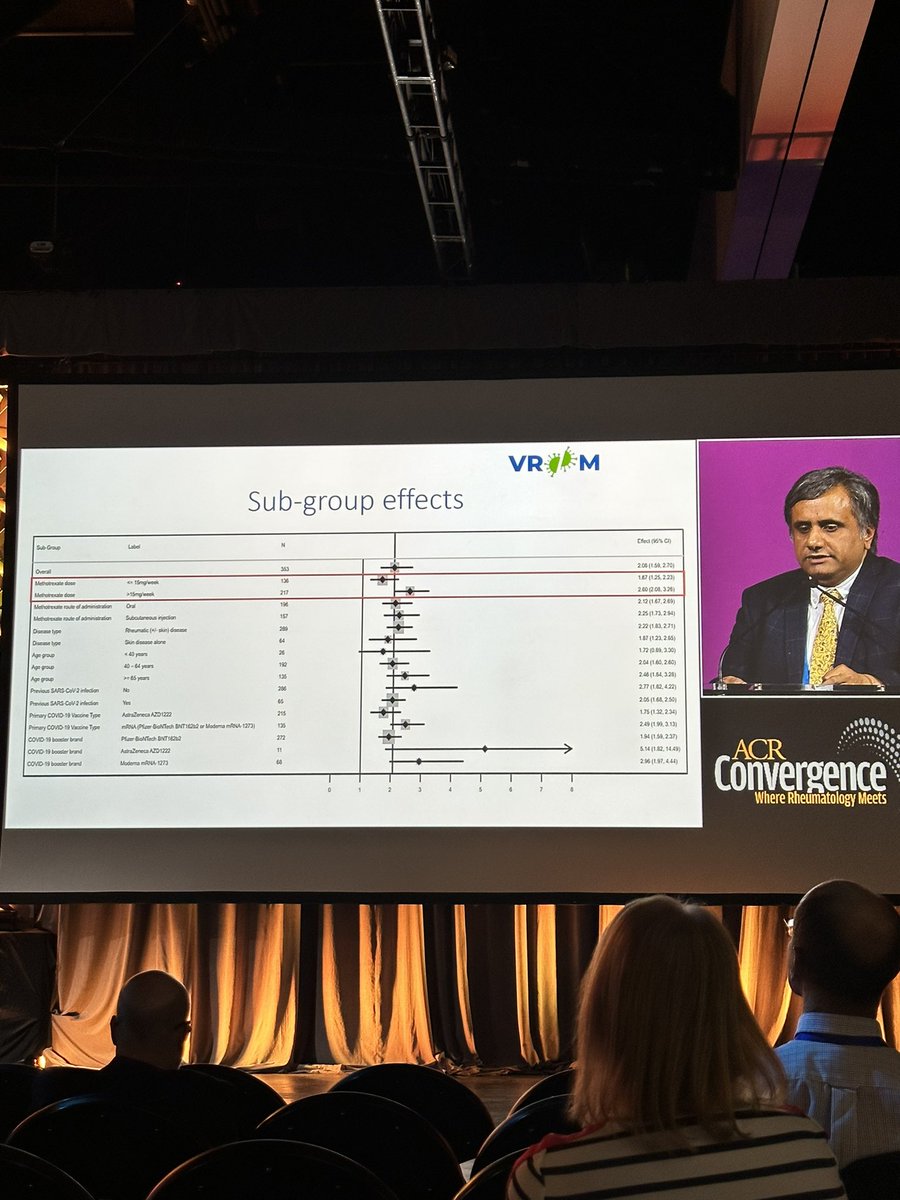
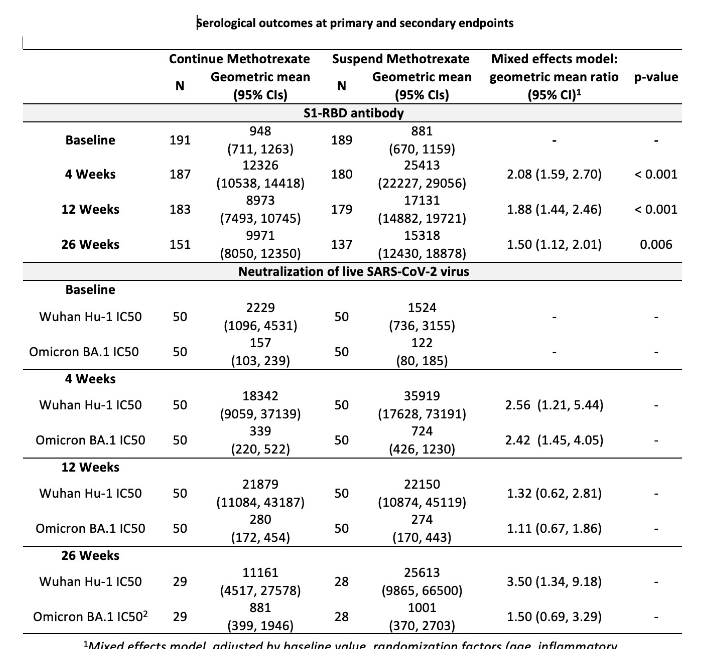
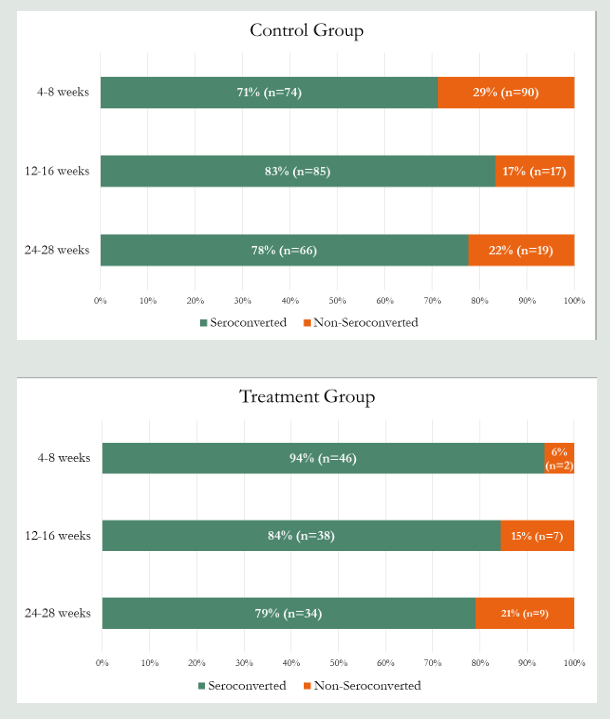
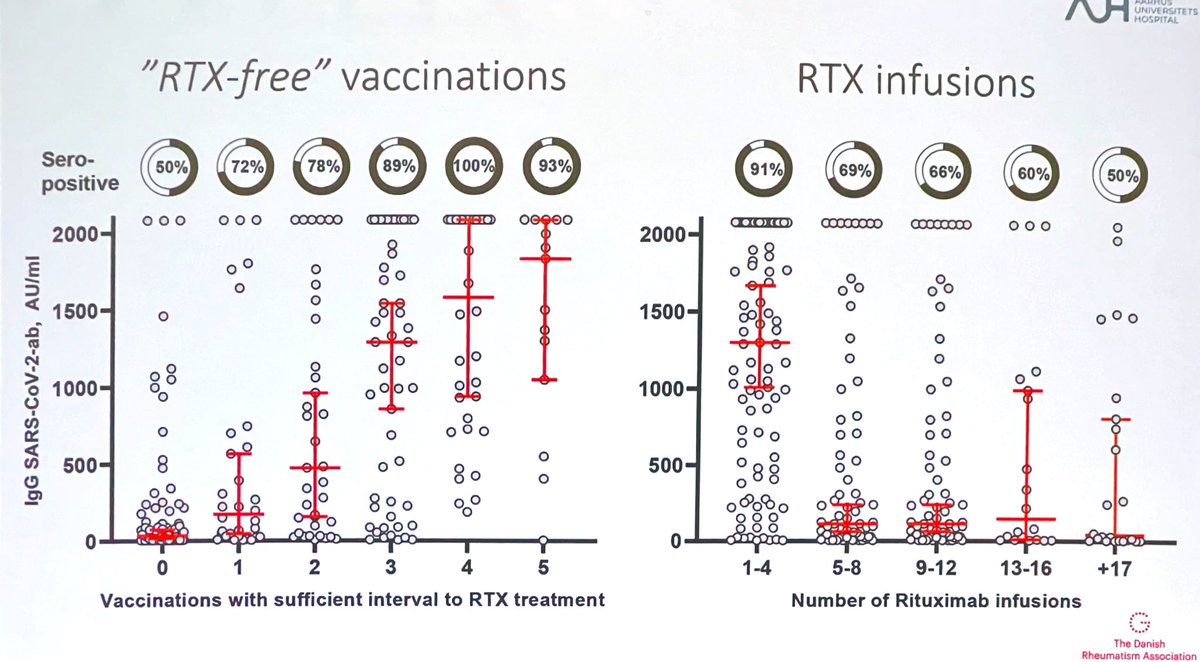
Nature Reviews Rheumatology features a review of three notable papers that address the impact of SARS-CoV-2 vaccination on people with inflammatory rheumatic disease.
Vaccine efficacy remains an important and highly discussed topic at this year’s annual meeting given the ongoing COVID-19 global health crisis, current influenza season, and recently published 2022 ACR guidelines for vaccinations in patients with rheumatic and musculoskeletal diseases.
Fast forward nearly 3 years since the first case of COVID-19 was reported, and I am amazed of the speed of response on how to keep our patients with rheumatic and musculoskeletal disease (RMD) safe from this infection.
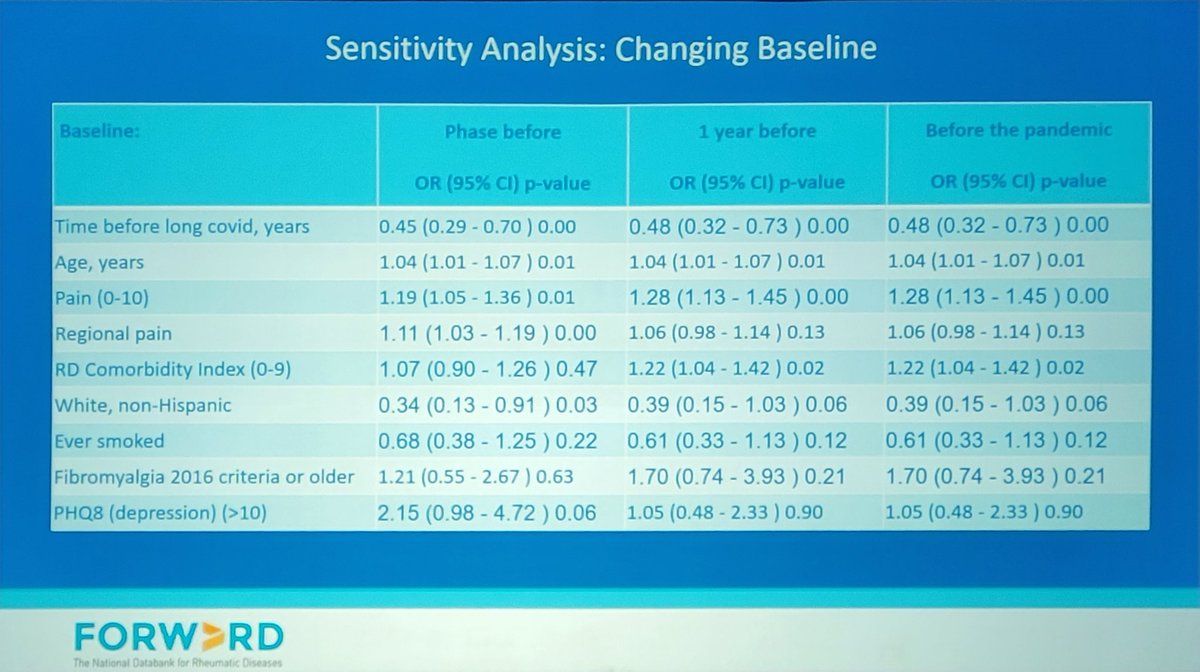
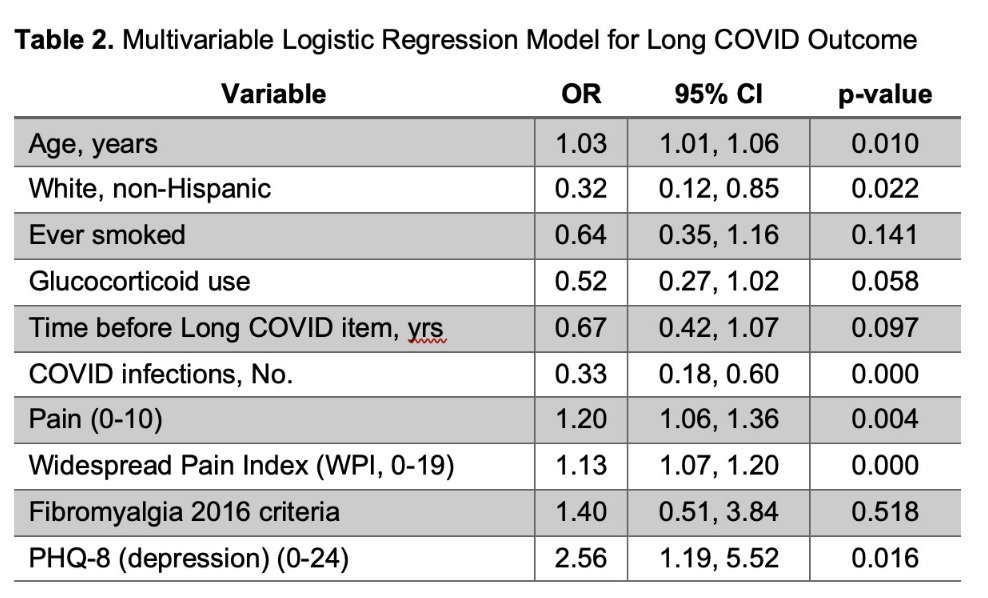
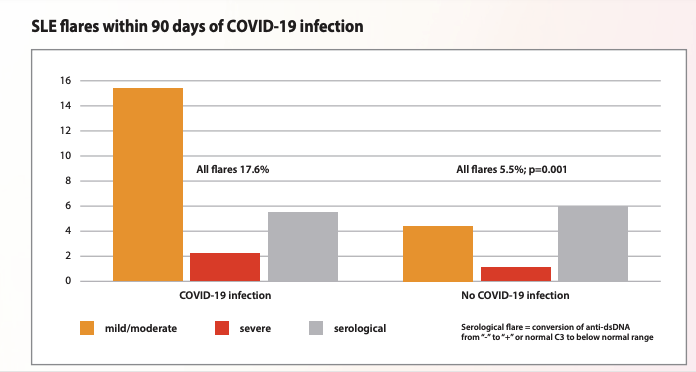
The COVID-19 pandemic has had a significant impact worldwide particularly among those who are immunocompromised. Numerous studies have highlighted the increased risk of acute SARS-CoV-2 infection among patients with rheumatic diseases (RD).

Jeffrey Sparks MD MMSc @jeffsparks ( View Tweet )

Dr. Antoni Chan ( View Tweet )