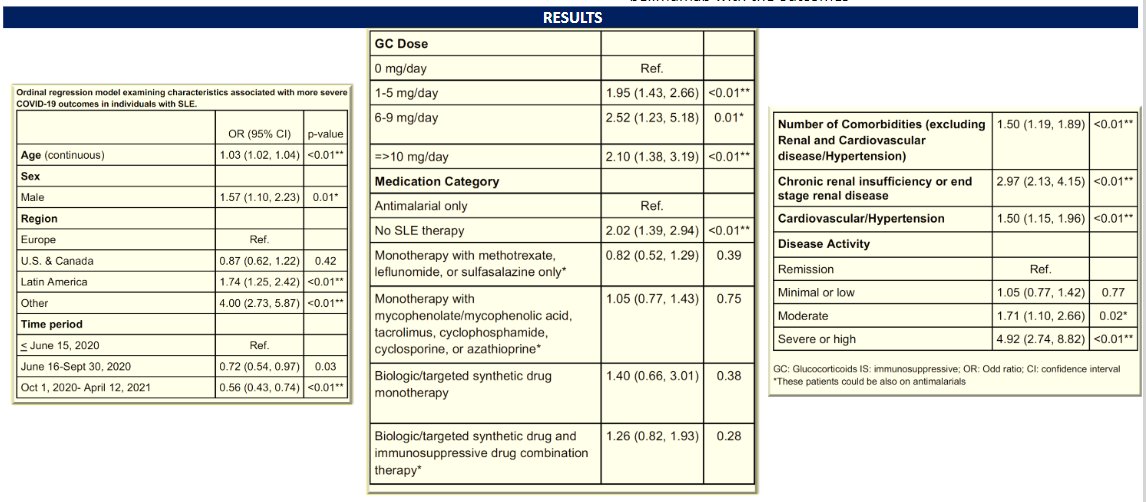
Plaquenil Does Not Protect Lupus Patients from COVID-19
Annals of Rheumatic Disease reports on an analysis of lupus (SLE) patients that shows COVID-19 infection rates were similar between those lupus patients who were taking hydroxychloroquine (HCQ) and those not taking HCQ.