"Don't You Know Who I am?" (5.17.2024)
Dr. Jack Cush reviews the news and journal reports from the past 2 weeks. This week's question: can we prevent gout, ILD or psoriasis?
Read ArticleDr. Jack Cush reviews the news and journal reports from the past 2 weeks. This week's question: can we prevent gout, ILD or psoriasis?
Read Article

Dr. John Cush @RheumNow( View Tweet )

Positive findings with color Doppler ultrasound were enough to diagnose giant cell arteritis (GCA) accurately without need for confirmation with temporal artery biopsy (TAB), a prospective study indicated.
Out of 165 older patients in whom GCA was strongly suspected, 73 (44%) had the
Read Article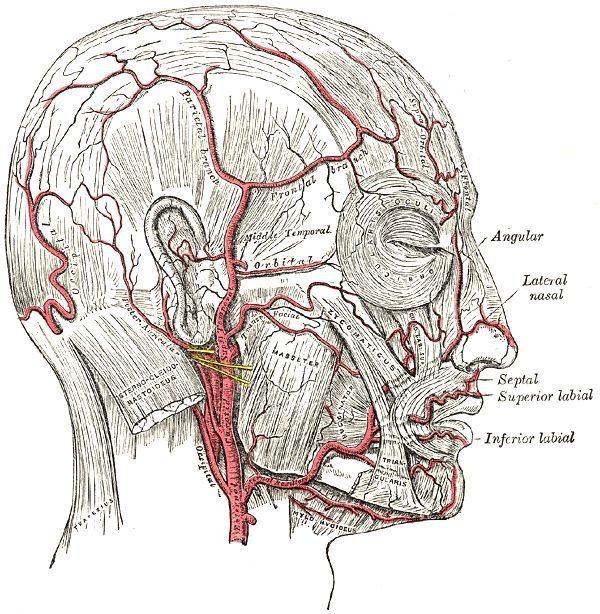
Dr. Jack Cush muses on the news, journal reports, FDA announcements and the 2024 BSR abstracts just released.
Read Article
Dr. Jack Cush reviews this past week’s news and journal articles from RheumNow.com.
Read Article

Dr. John Cush @RheumNow( View Tweet )

Dr. John Cush @RheumNow( View Tweet )

Dr. John Cush @RheumNow( View Tweet )
Dr. Jack Cush reviews regulatory reports, news and novel journal articles - this week focusing on Sjogren's, ILD, Gout and Uveitis.
Read Article
Dr. John Cush @RheumNow( View Tweet )

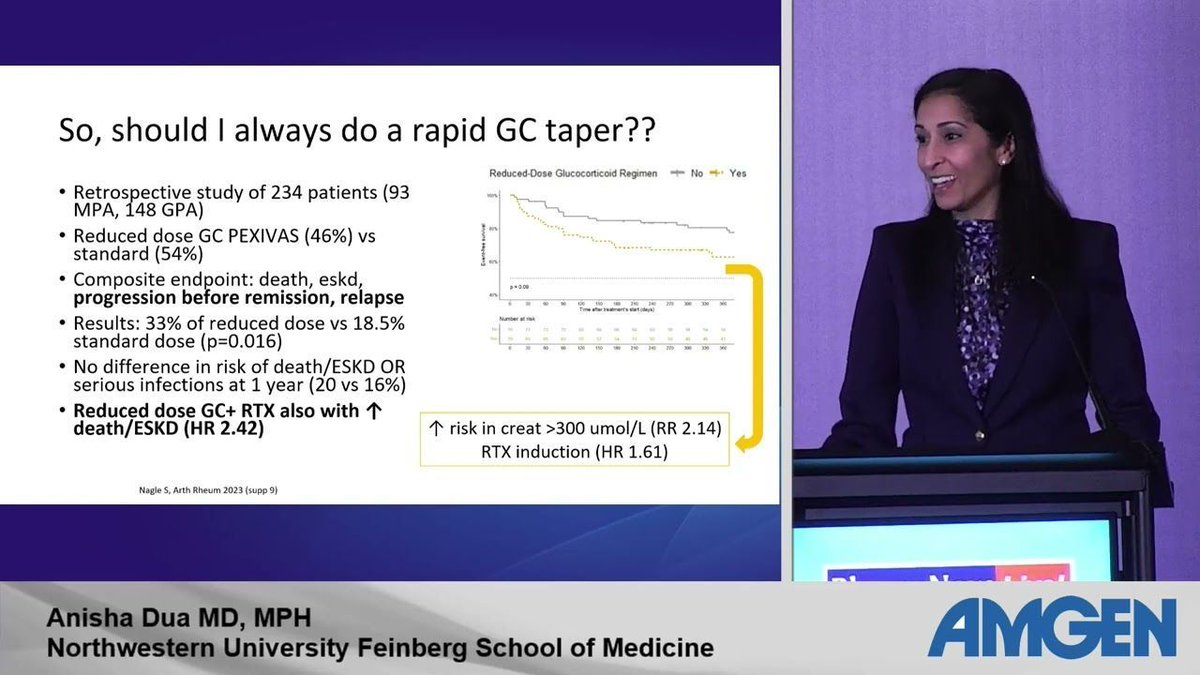
Once again RheumNow Live 2024 really delivered with high impact learning packed into short sessions. As someone with an interest in vasculitis it was fantastic to see four of my favorite speakers in the Vasculitis Mavens and STEP talks. They gave us what we really want from these talks –
Read Article
Links:

Imaging is often instrumental in diagnosing and staging patients diagnosed with giant cell arteritis (GCA). A new study compared the diagnostic performance of Colour Duplex Ultrasound (CDUS), Fluor-18-deoxyglucose Positron Emission Tomography Computed Tomography (FDG-PET/CT) and
Read Article
Epidemiologic studies of Henoch-Schönlein purpura (HSP) have suggested seasonal variation in occurrence rates (higher from September-April, lower in June-August), suggesting a role for infectious triggers. The importance of infection was recently shown with nonpharmaceutical interventions (
Read Article