Lupus

Richard Conway RichardPAConway
3 years 2 months ago
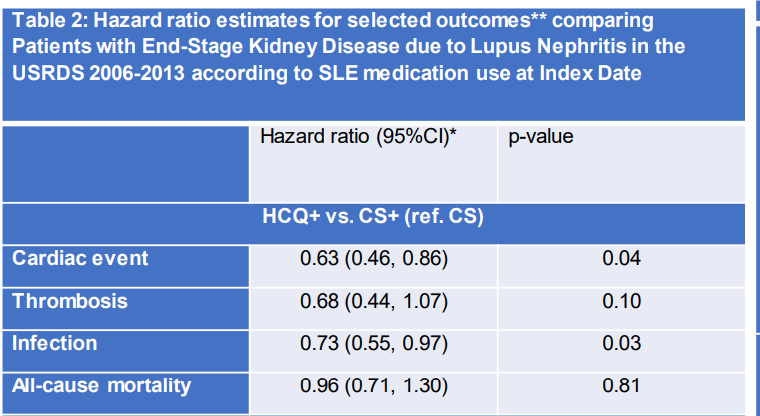
Broder et al. HCQ alone vs steroid alone as maintenance in ESKD due to SLE. HCQ less cardiac events, less infection. @RheumNow #ACR22 Abstr#0539 https://t.co/mb3Eof2Uiv https://t.co/3i3ZTY25ru

Eric Dein ericdeinmd
3 years 2 months ago
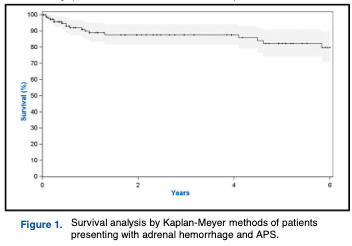
Ab0676 #ACR22 Adrenal hemorrhage in APLS
59 pts from SLE cohort + 181 from lit review
65% prior VTE, 12% CVA, 24% OB morbidity
46% thrombocyt, 21% had SLE
58% on a/c
69% b/l hemorrhage
63% adrenal insuff
Radiol remission: 6% at 1 yr, 41% at 5yr
Death 2% 1 yr, 11% at 5
@RheumNow https://t.co/EacifcN7Sd

Eric Dein ericdeinmd
3 years 2 months ago
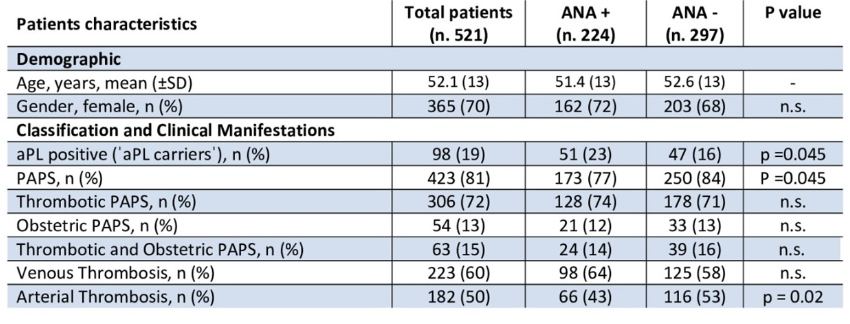
Ab0683 #ACR22
aPL Pts ANA pos vs neg:
521 pts with +aPL Ab WO other autoimmune disease
224 +ANA, 297 -ANA
ANA+ ass w/ hemolytic anemia, thrombocyt, leukopenia, livedo, unexplained fetal death
Trend for arthritis, aPL nephropathy
@RheumNow https://t.co/3NHGymyL1C

Eric Dein ericdeinmd
3 years 2 months ago
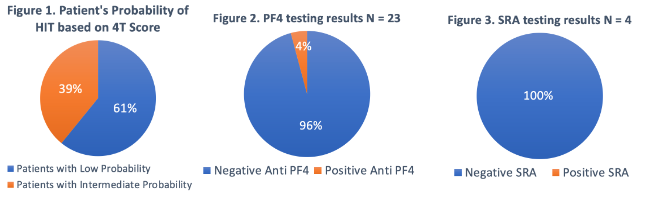
Ab0674 #ACR22 HIT AND APLS??
Retrosp review of 23 pts treated for HIT in the hospital with APLS or SLE with aPL Ab:
Not one ultimately met clinical criteria for HIT
1 pt had PF4 antibodies, SRA testing negative in ALL cases
Thrombocytopenia w/ aPL Abs? Think APS 1st!
@Rheumnow https://t.co/ZYZP5VZF0R

Richard Conway RichardPAConway
3 years 2 months ago
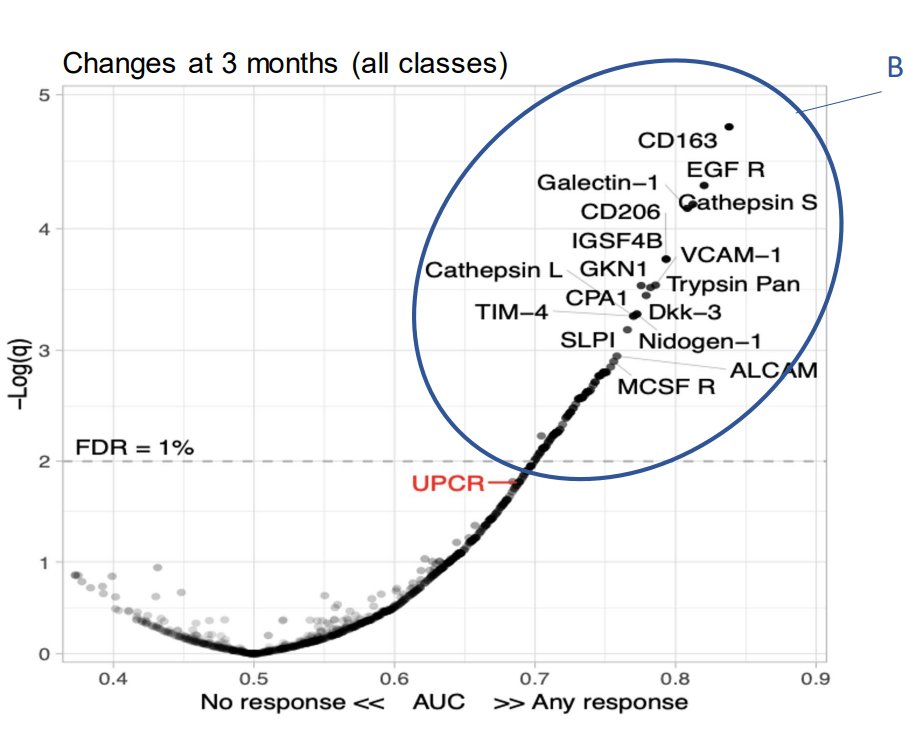
Fava et al. Urinary biomarkers at 3 months better than UPCR in predicting 12 month treatment response in SLE nephritis . CD163 AUC 0.83 vs 0.75 for UPCR @THKC1 @RheumNow #ACR22 Abstr#0536 https://t.co/YI3JC2uKcv https://t.co/jnkfbI0Z1M

Md Yuzaiful Md Yusof Yuz6Yusof
3 years 2 months ago
Here is a quick recap on #ACR22 Abstr#0355 Effect of voclosporin in class V lupus nephritis #lupus https://t.co/0cR8On5UWN via @YouTube @RheumNow https://t.co/E25so6X2fj

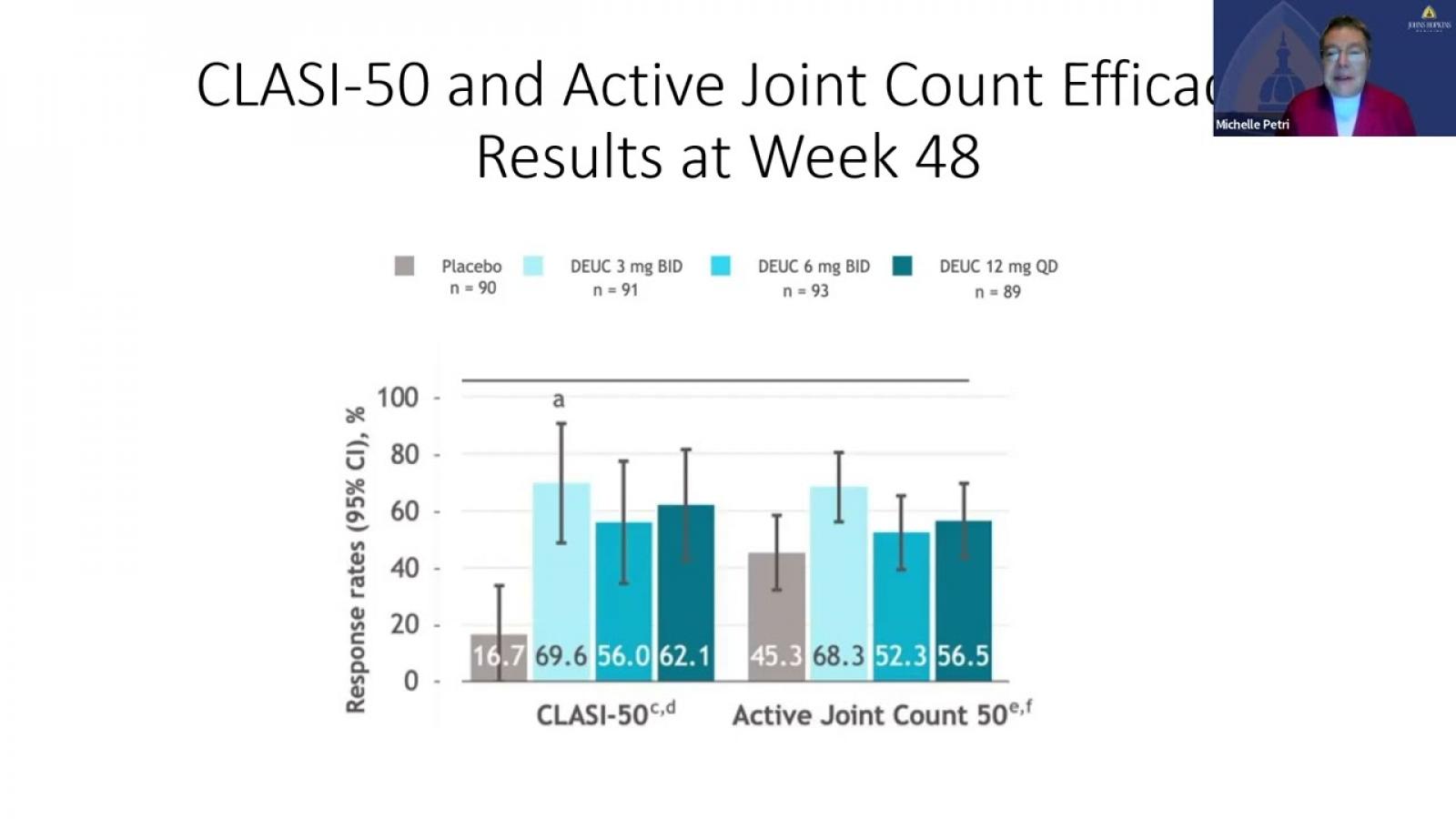
Dr. Rachel Tate uptoTate
3 years 2 months ago
Preliminary results anifrolumab may be effective in highly recalcitrant & RTX resistant CLE and DLE. Abs 0974 #ACR22 @RheumNow https://t.co/FeYrdlwQsA

Richard Conway RichardPAConway
3 years 2 months ago
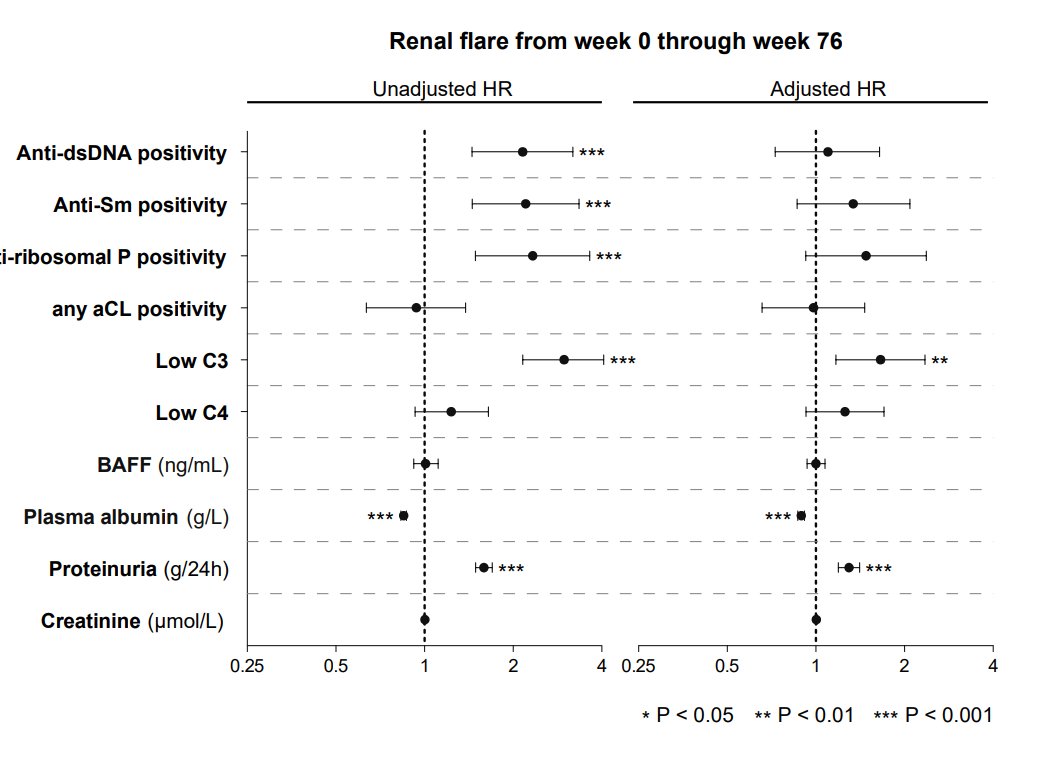
Gomez et al. Predictors renal flare in SLE. Adjusted models - low C3, low albumin, proteinuria. @RheumNow #ACR22 Abstr#0540 https://t.co/POfeAa9Ao9 https://t.co/a3JkSP1MkX

Richard Conway RichardPAConway
3 years 2 months ago
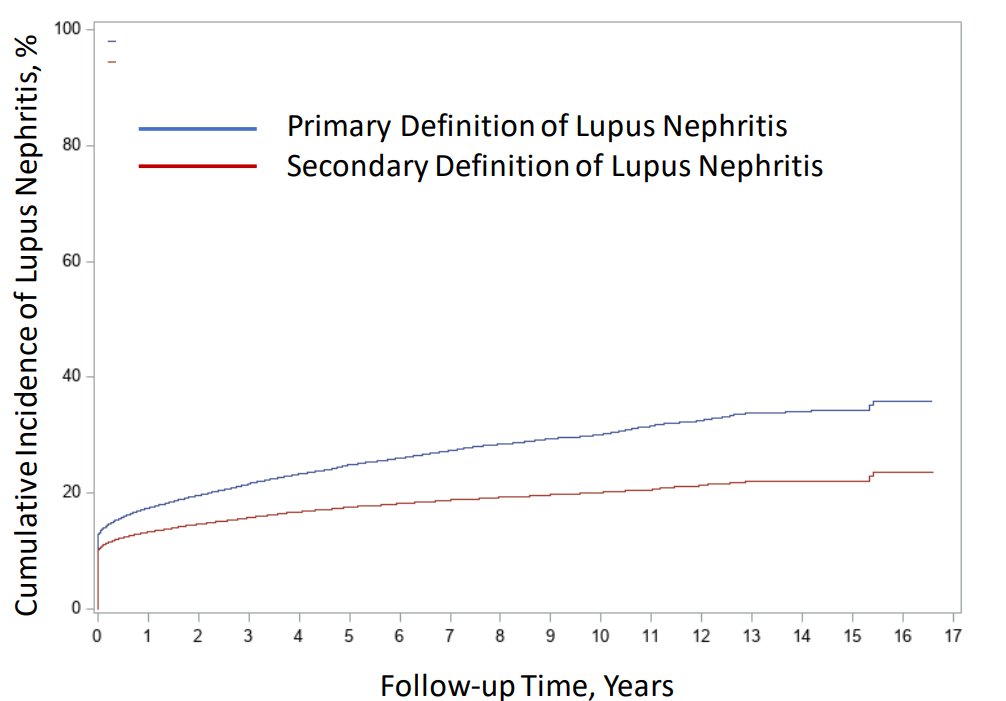
Jorge et al. @AprilJorgeMD Incidence SLE nephritis - 16% onset, 35% 15 years. 44.7% men vs 28.6% women at 10 years. 40% Black, 38% Hispanic, 40% Asian, 23% White. @RheumNow #ACR22 Abstr#0538 https://t.co/Nbx16jZAN7 https://t.co/BEnAtbcIHt

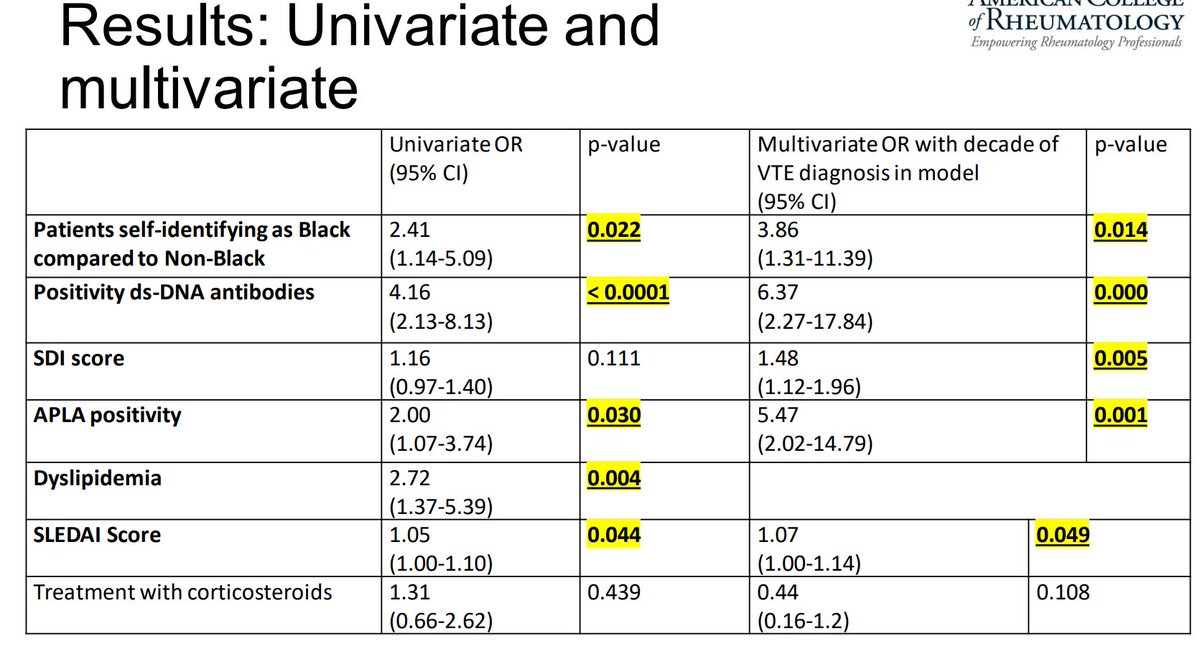
Richard Conway RichardPAConway
3 years 2 months ago
Tofighi et al. VTE in SLE nephritis. 10% VTE, 5.2% VTE after SLE nephritis diagnosis. Risks - Black patients, ds-DNA+, SDI, aPL+, SLEDAI. @RheumNow #ACR22 Abstr#0541 https://t.co/G6q0qvirf7 https://t.co/B8STBTMy14

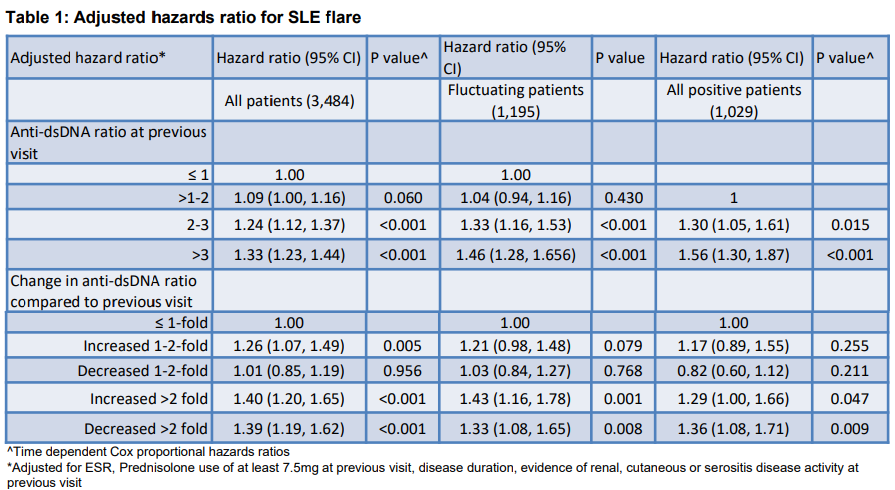
sheila RHEUMarampa
3 years 2 months ago
Interesting study by Dr Ai Li Yeo and colleagues on repetitive anti-dsDNA testing and flare prediction:
🔅Fluctuations (⬆️and ⬇️) in anti-dsDNA >2 fold was assoc'd w/⬆️flares in all groups including persistently + pts.
#ACR22 @RheumNow ABST#327 https://t.co/q0WXnIwV4A

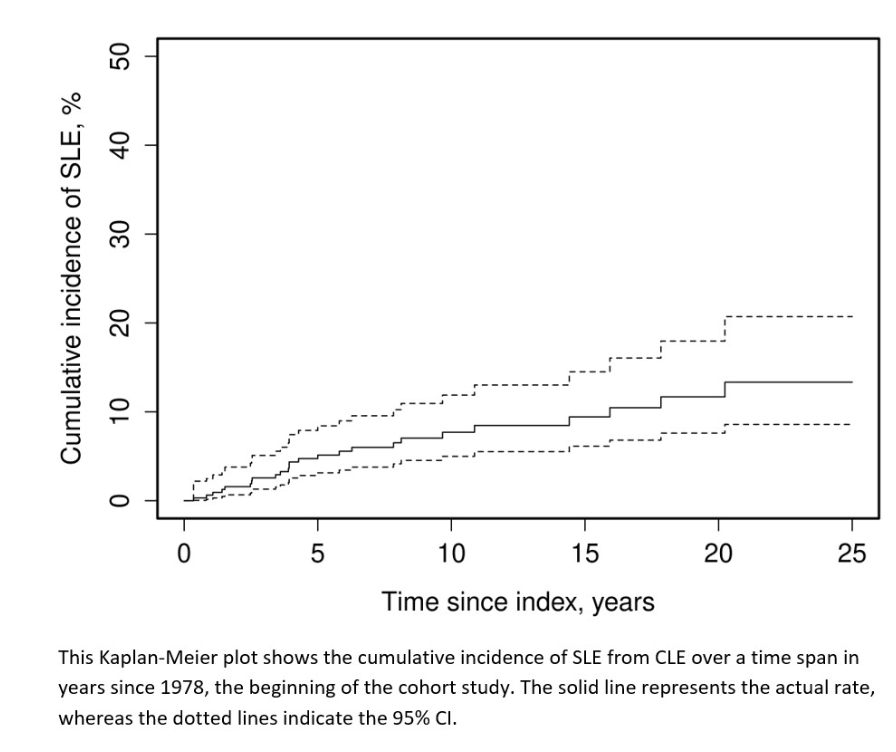
Eric Dein ericdeinmd
3 years 2 months ago
Abst0338 #ACR22 Transition from CLE to SLE
324 cases of incident cutaneous lupus, mean f/u 8 years
26 pts developed SLE. 5.2% transition by 5 years, <3% risk every 5 yrs from 5-20 years
Risk factors: SCLE, younger age, recent diagnosis
@RheumNow #ACRBest https://t.co/JFcUIkfA9n














 Poster Hall
Poster Hall