Psoriatic arthritis

Dr. Antoni Chan synovialjoints
3 years 2 months ago
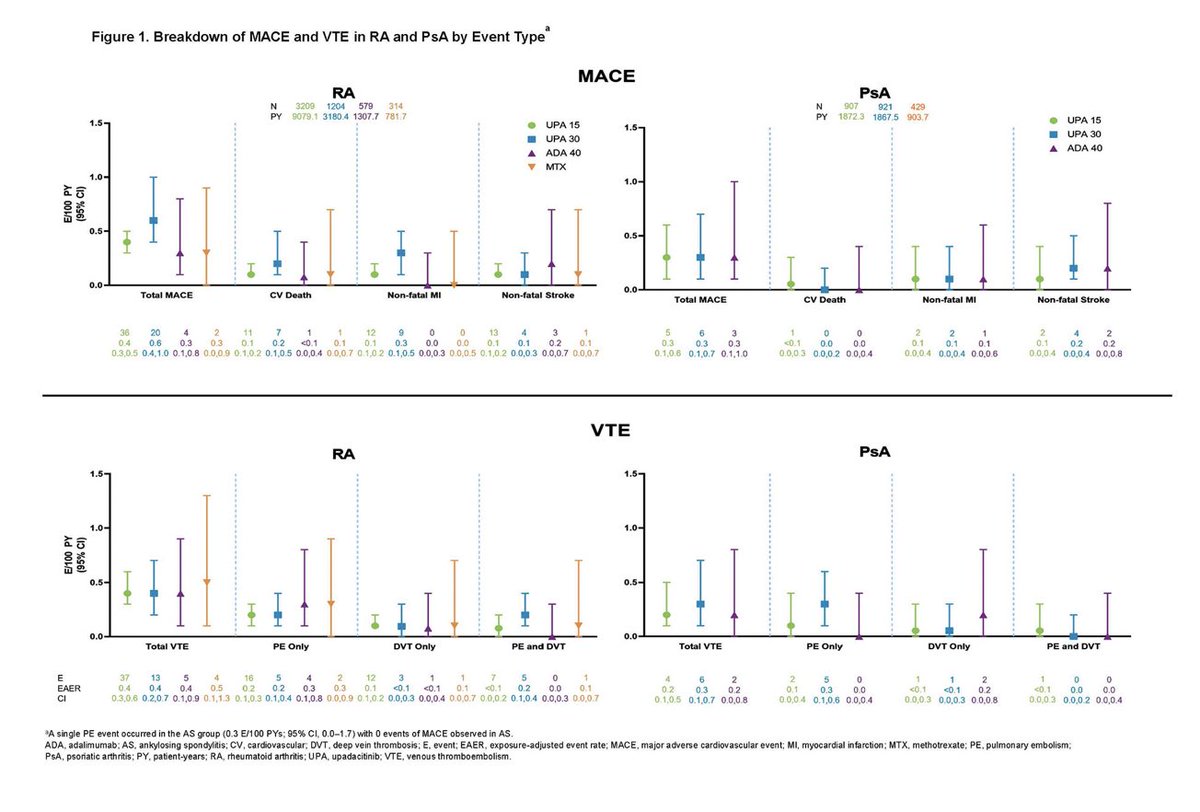
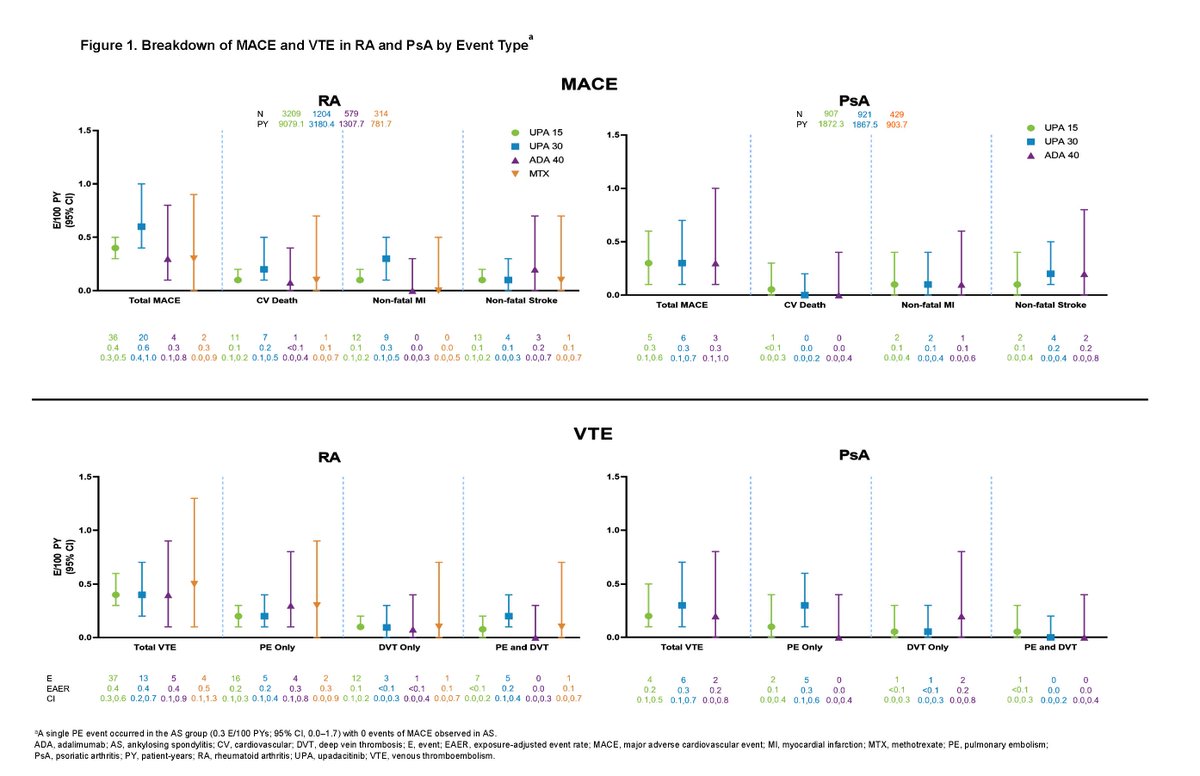
Across 9 trials of Upadacitinib in RA, PsA and AS, 40%–50% of patients had ≥ 2 CV risk factors, ≥ 65 years 6%–23%. Rates of adjudicated MACE and VTE with UPA were infrequent, consistent with background rates in RA, PsA, and AS Abst 0510 https://t.co/HDkQ6ELnAy #ACR22 @RheumNow https://t.co/SRJYdFFNIQ

sheila RHEUMarampa
3 years 2 months ago
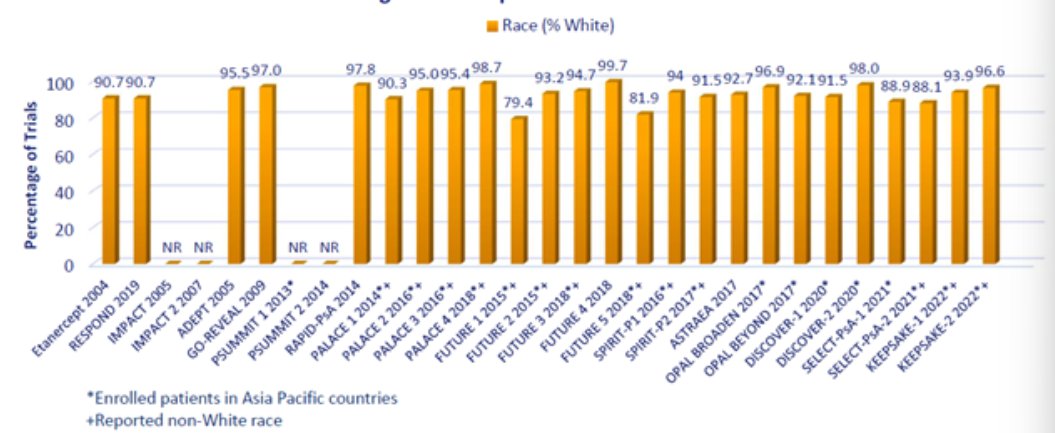
In this study, Dr. Niti Goel shows the under-reporting of race & ethnicity in publications of #psoriaticarthritis clinical trials
🧐Participant diversity is important to consider since different races & ethnicities may respond differently to therapies
#ACR22 @RheumNow ABST0090 https://t.co/BzHpuHYVI5

sheila RHEUMarampa
3 years 2 months ago
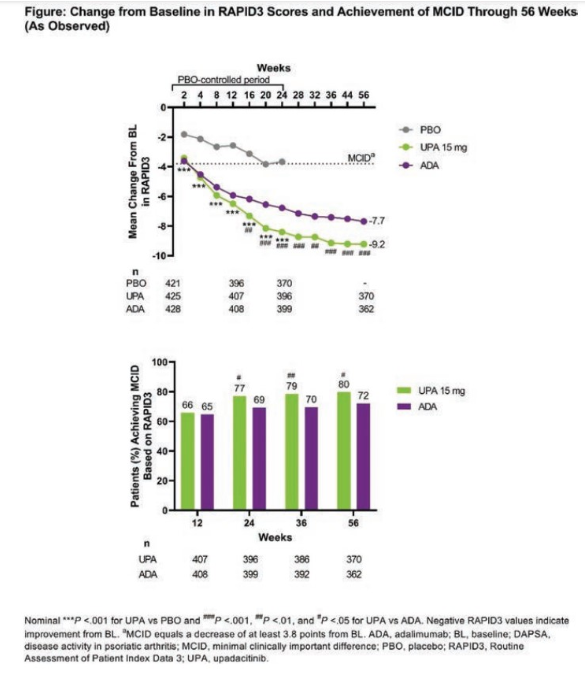
Post hoc analysis from the SELECT-PsA 1 trial by Dr. @DrLauraCoates and team:
💊Pts on UPA showed greater improvement from BL in RAPID3 vs. ADA in all visits
💊Pts on UPA had better responses in all assessments vs. PBO
Reassuring data. #ACR22 @RheumNow ABST0192 https://t.co/NgeUU5bPPf
It’s widely accepted that Psoriatic disease has multi-system, multi-domain potential that can lead to life altering complications if left untreated or undertreated. Rheumatologists have shifted the way we discuss treatment options and disease state expectations with patients. Two #ACR22 abstracts stood out to me regarding the Psoriatic disease patient experience and will, ultimately, add to what I do in clinic.

Patricia Harkins DrTrishHarkins
3 years 2 months ago
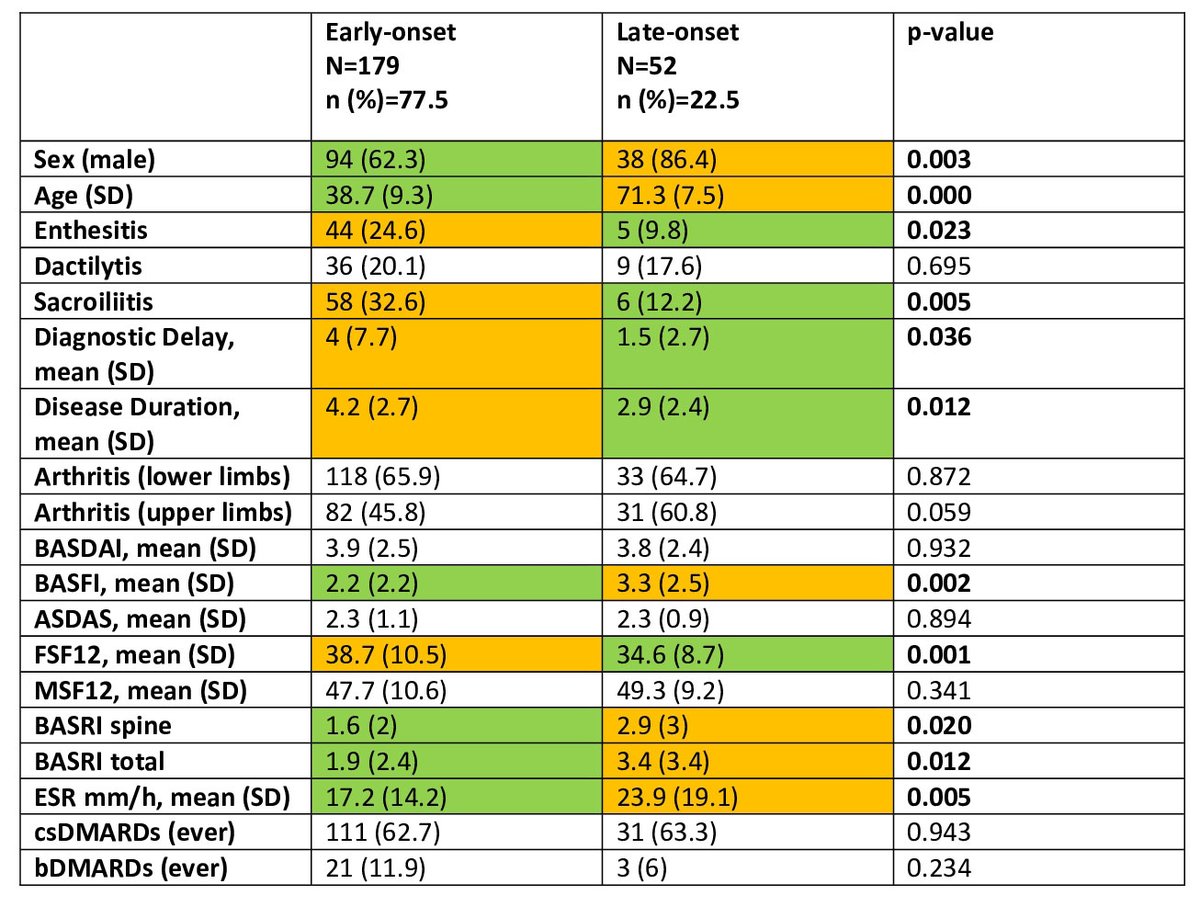
🤕 Late onset PsA associated with
⬆️ structural damage
💪🏻UL > LL arthritis
⬆️ BASFI
🙋♂️ males
⬇️ enthesitis/ sacroilitis
Abst# 0377
#ACR22 @RheumNow

Catherine Sims, MD DrCassySims
3 years 2 months ago
What’s new to treat PsA? Let’s discuss anti-IL-17A, Izokibep #ACR22 @RheumNow
Abstract #0199
💪 Izokibep 40 v. 80 mg q2 weeks SQ v. placebo
💪 135 patients, 28 sites
💪 At 12 weeks, all patient reported outcomes and PsAID subdomains significantly improved (dose dependent)

Dr. Rachel Tate uptoTate
3 years 2 months ago
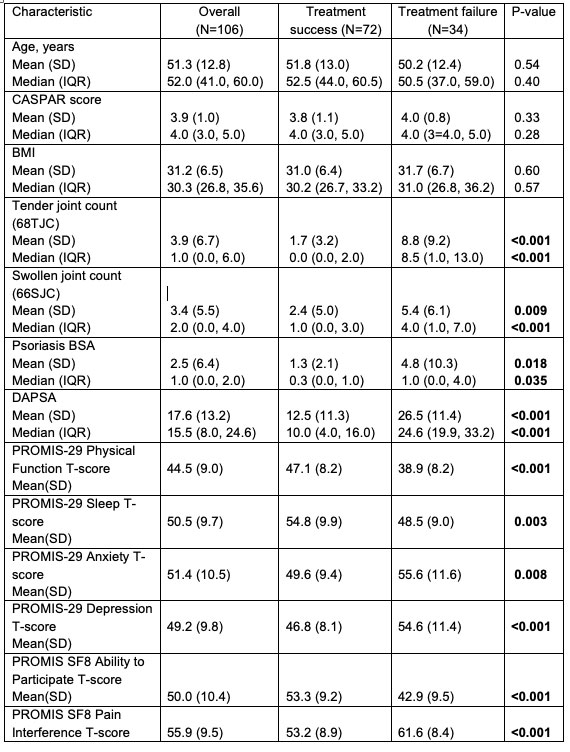
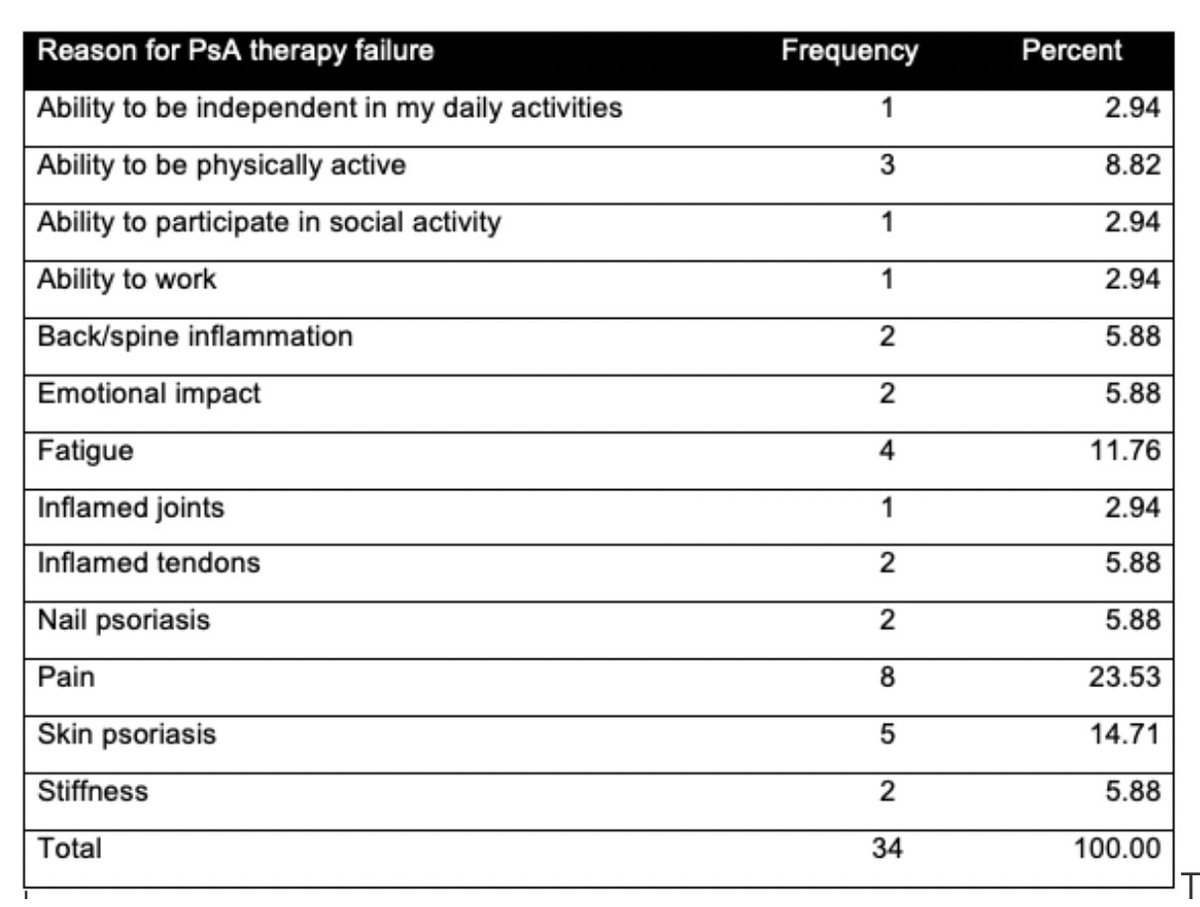
Clinical pearl! Patient-reported treatment success in PsA assoc'd w/ control of arthritis, dactylitis, psoriasis, and health-related QoL. Top 3 pt-reported reasons for tx failure were pain, psoriasis and fatigue. Abs0393 #ACR22 @RheumNow https://t.co/F9RNI7EXcL https://t.co/7DcLaqUqnm

Robert B Chao, MD doctorRBC
3 years 2 months ago
Rates of MACE and VTE with upadacitinib were infrequent and consistent with background rates in RA, PsA and AS patients. Factors associated with MACE/VTE: age>65, HTN, DM, smoking, history CV event/VTE
Abs#0510 @RheumNow #ACR22 https://t.co/AjtJF0p3QK

Aurelie Najm AurelieRheumo
3 years 2 months ago
Do you consider ttmt successful? Question Christeen et al. asked to 100+ PsA pts. 1/3 pts said no, they had > TJC, > SJC, > Pso & > dactylitis.
Failure also w/: pain 24%, pso 15%, fatigue 12% and < ability to be active 9%.
https://t.co/dQseCNSDBS Abstr #0393 #ACR22 @Rheumnow https://t.co/kGlmscsKL7

Dr. Rachel Tate uptoTate
3 years 2 months ago
Interesting observation: Late-onset PsA assoc'd w/ male sex, greater structural damage, higher frequency of arthritis, and greater loss of functionality (BASFI). Interestingly, shorter time of symptom duration to dx. Abs 0377 #ACR22 @RheumNow https://t.co/m15c37FltD https://t.co/3LRy4Ltde6


















 Poster Hall
Poster Hall