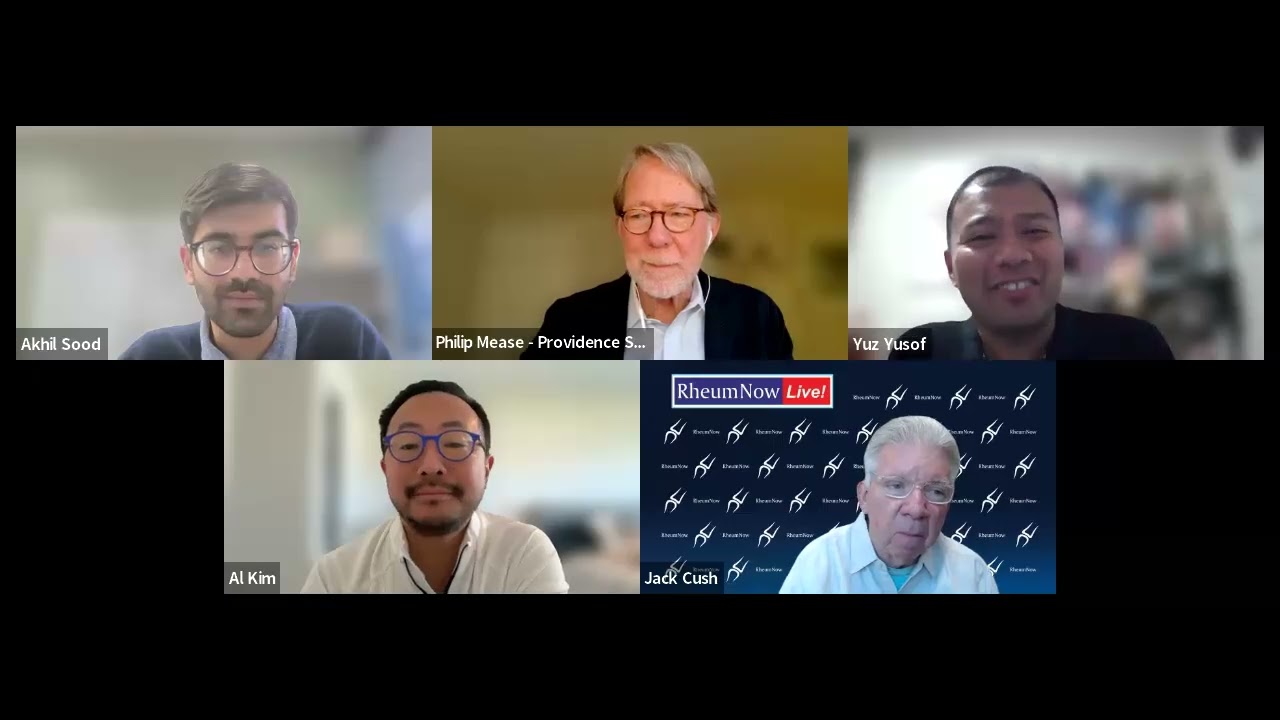
ACR2025 CAR-T Topic Panel
A focused conversation on the latest in CAR-T from emerging data and treatment strategies to real-world challenges in diagnosis and management. Hear expert perspectives, clinical pearls, and what’s shaping CAR-T practice right now. Panelists: Drs. Al Kim, Philip Mease, Yuz Yusof, Akhil Sood, and Jack Cush.
Watch video →






























 Poster Hall
Poster Hall