Polymyalgia Rheumatica: An Interval Look at Management Questions Save
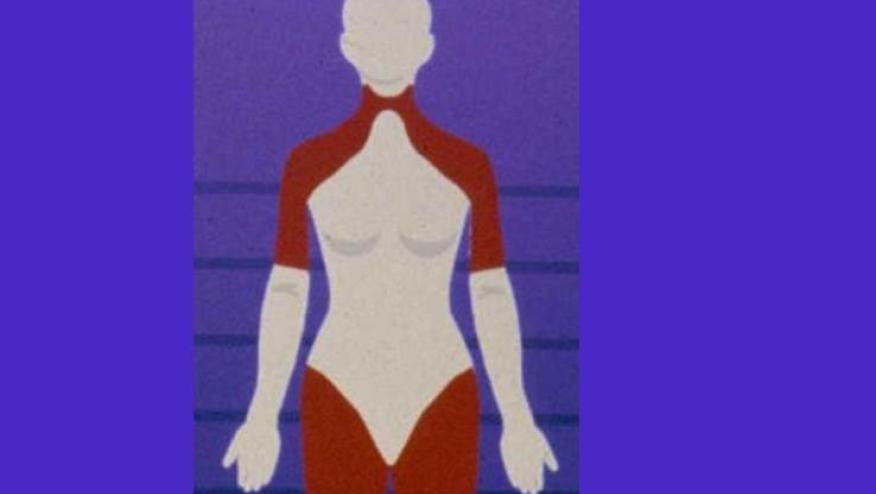
New onset bilateral shoulder pain, stiffness, functional impairment, and constitutional symptoms such as fatigue, night sweats, weight loss, and fever are characteristic clinical features of polymyalgia rheumatica (PMR), the second most common inflammatory rheumatic disease of older people. Inflammatory markers are elevated in the vast majority of cases; therefore, the diagnosis of PMR must be questioned if both, ESR and CRP are normal. Despite this often fairly characteristic pattern of signs and symptoms, there are significant diagnostic challenges in this disease. The reason is that similar clinical features can be also observed in other diseases mimicking PMR including infectious and malignancies, elderly-onset rheumatoid arthritis, giant cell arteritis, chondrocalcinosis or myositis, to mention some of the most important differential diagnoses.
MRI and PET imaging: helpful in characterization and management
Imaging techniques such as ultrasound, magnetic resonance imaging (MRI), and to some extent 18F-fluorodeoxyglucose positron emission tomography (18F-FDG-PET), are increasingly used to support the diagnosis of PMR, to rule out differential diagnoses and/or to assess response to therapy. For example, ultrasound detection of characteristic subdeltoid bursitis, biceps tenosynovitis and/or glenohumeral/hip synovitis may help to improve diagnostic accuracy of PMR whereas the deposition of calcium pyrophosphate in the hyaline cartilage of these joints suggests chondrocalcinosis as an alternative diagnosis.
Very recently, Mackie et al. have identified in a MRI study a subset of PMR patients with an extracapsular pattern of inflammation [1]. This includes periacetabular inflammation extending from the anterior hip capsule, medial to gluteus minimus and lateral to the iliac bone. It also includes inflammation inferior to the symphysis pubis, but did not involve the synovial hip joint. Most interestingly, the involvement of these periarticular structures turned out to be a powerful predictor of response to glucocorticoid therapy. Moreover, this pelvic involvement seems to represent a feature which could aid in the distinction between PMR and rheumatoid arthritis.
These observations underline the current view that the disorder we currently call PMR does not seem to represent a homogeneous disease. Rather, there seem to be existing pathophysiological variants or even different diseases, perhaps requiring different therapeutic approaches. Given this background, we expect imaging techniques to increasingly support diagnosis and differential diagnosis procedures in PMR in the near future. For example, while MRI is currently not recommended for daily clinical practice in every patient with PMR, it is considered to be useful in cases of diagnostic uncertainty. Also, we expect study data in the future to inform the relevance of initial and follow-up MRI imaging for prognosis and treatment decisions, as well as studies investigating the cost-effectiveness of this technique for PMR management [2].
Similar considerations apply to the use of 18F-FDG-PET (most often combined with low-dose computed tomography) in the context of PMR. This technique detects not only inflammation of shoulders, hips and other joints, but also (subclinical) large vessel vasculitis and other diseases, and is therefore valuable for PMR cases with overlapping giant cell arteritis, or, like MRI, in cases of diagnostic uncertainty. This technique is likely to open new avenues for answering diagnostic, prognostic and treatment questions as our knowledge and insights about PMR evolve.
Treatment considerations:
At a review during the 2015 ACR annual meeting, one of us (ELM) asked for a show of hands of how many in the large audience of over 500 attendees prescribed methotrexate ad adjuvant treatment for PMR. Since I rarely use methotrexate for PMR, and my personal “guidelines” for doing so are admittedly less than systematic, I was rather surprised to see that about 80% of the audience raised their hands.
The only established therapy for PMR is glucocorticoids. With the often protracted disease course of PMR, glucocorticoid (GC) adverse effects are very common and often associated with significant morbidity, especially osteoporosis, diabetes and cataracts.
Consensus-based recommendations, including the recently released 2015 ACR-EULAR management recommendations, uniformly consider GCs as therapy of choice for PMR [3]. The guidelines suggest initiation of treatment with prednisone equivalent, 12.5 to 25 mg a day, reflecting the uncertainty regarding best dosing practices.
There are actually just 2 randomized clinical trials which have evaluated GC GC dosing regimens for PMR in the absence of GCA. A small (39 patient) open study compared 10 mg/day vs 20 mg a day oral prednisone for PMR and found that patients treated with the higher dose had a lower relapse rate at 2months following initiation of therapy [4].
In Great Britain, the efficacy and safety of intramuscular (i.m.) methylprednisolone at a dose of 120mg every 3 weeks was compared to 15mg/day oral prednisone in a 96-weeks double blinded randomized trial. Overall, remission rates were comparable between the two doses, however patients receiving the i.m. dosing had lower cumulative GC dose over the study period, with less weight gain [5,6]. Based on these results, i.m. methylprednisolone may be considered as a treatment alternative in patients with PMR, but this regimen has not been adopted with any regularity by any clinic or practice we are familiar with.
Methotrexate and other disease modifying anti-rheumatic drugs (DMARDs)
The possible benefit of methotrexate as a GC sparing drug has been reported from 2 RCTs . One of these was a multicenter double blinded study with random treatment assignment over 76-weeks. The investigators reported that patients on methotrexate had somewhat fewer relapses, received a lower cumulative GC dose, and were more likely to discontinuation use of GCs [7]. No safety advantage was noted, as GC related adverse events were similar in both groups. The second study was an open label multicenter study in which subjects received methotrexate for the 12-months of the study period. As in the blinded RCT, these investigators reported that subjects receiving methotrexate had a lower cumulative dose of GC, lower relapse rate, and were more likely to discontinue GCs during the 12 months of the study. [8]. A factor which may have biased the outcome towards the methotrexate intervention is that the initial oral prednisone dose in the methotrexate groupwas 25 mg/day compared to 15 mg/day in the control group.
Evidence from these RCTs suggests that it may be that early introduction of methotrexate for treatment of PMR is beneficial, although it is uncertain if the putative beneficial effects are sustained over time, nor is it clear if initiation of methotrexate in patients with established PMR is beneficial. The use of other DMARDs is not supported by current evidence.
Biologics
Use of a number of biologics has been reported anecdotally, with IL-6 therapies generating the most enthusiasm. To date, however, only tumor necrosis factor-alpha (TNF-α) blocking agents have been systematically evaluated in RCT. Studies on infliximab and etanercept, however, failed their primary efficacy endpoints [9,10].
In summary, there are no high quality trials on initial GC dose, GC administration routes or tapering regimens in PMR. Available studies are mainly limited by insufficient blinding and selective outcome reporting. Clinical practice recommendations are thus mostly consensus-based and suggest an individualized GC treatment plan. New, more effective therapies are desperately needed for the management of PMR.
The optimal follow-up strategy for patients on treatment is not established, but the assessment of response to therapy in PMR should continue to be primarily based on clinical and laboratory findings. The utility of serial US, MRI or 18F-FDG-PET examinations has not been demonstrated./span/span/p div p dir="ltr"strongspan style="font-size:11px;"References/span/strong/p p dir="ltr"span style="font-size:11px;"1.nbsp;nbsp; nbsp;Mackie SL, Pease CT, Fukuba E, et. al. Whole-body MRI of patients with polymyalgia rheumatica identifies a distinct subset with complete patient-reported response to glucocorticoids. Ann Rheum Dis. 2015;74(12):2188-92. /span/p p dir="ltr"span style="font-size:11px;"2.nbsp;nbsp; nbsp;Buttgereit F, Matteson EL. Imaging: Whole-body MRI undresses polymyalgianbsp;rheumatica. Nat Rev Rheumatol. 2016;12(3):140-1/span/p p dir="ltr"span style="font-size:11px;"3. nbsp;nbsp; nbsp;Dejaco C, Singh YP, Perel P, al e. Recommendations for management of polymyalgia rheumatica: an European League Against Rheumatism and American College of Rheumatology collaborative initiative. a href="http://www.ncbi.nlm.nih.gov/pubmed/26352874"Arthritis Rheum/a 2015; 67(10):2569-80 and a href="http://www.ncbi.nlm.nih.gov/pubmed/26359488"Ann Rheum Dis./a 2015 Oct;74(10):1799-807. /span/p p dir="ltr"span style="font-size:11px;"4.nbsp;nbsp; nbsp;Kyle V, Hazleman BL. Treatment of polymyalgia rheumatica and giant cell arteritis. I. Steroid regimens in the first two months. Ann Rheum Dis 1989;48(8):658-661./span/p p dir="ltr"span style="font-size:11px;"5.nbsp;nbsp; nbsp;Dasgupta B, Dolan AL, Panayi GS, Fernandes L. An initially double-blind controlled 96 week trial of depot methylprednisolone against oral prednisolone in the treatment of polymyalgia rheumatica. Br J Rheumatol1998;37(2):189-195./span/p p dir="ltr"span style="font-size:11px;"6.nbsp;nbsp; nbsp;Dolan AL, Moniz C, Dasgupta B, et al. Effects of inflammation and treatment on bone turnover and bone mass in polymyalgia rheumatica. Arthritis Rheum 1997;40(11):2022-2029./span/p p dir="ltr"span style="font-size:11px;"7.nbsp;nbsp; nbsp;Caporali R, Cimmino MA, Ferraccioli G, et al. Prednisone plus methotrexate for polymyalgia rheumatica: a randomized, double-blind, placebo-controlled trial. Ann Intern Med 2004;141(7):493-500./span/p p dir="ltr"span style="font-size:11px;"8.nbsp;nbsp; nbsp;Ferraccioli G, Salaffi F, De Vita S, Casatta L, Bartoli E. Methotrexate in polymyalgia rheumatica: preliminary results of an open, randomized study. J Rheumatol 1996;23(4):624-628./span/p p dir="ltr"span style="font-size:11px;"9.nbsp;nbsp; nbsp;Kreiner F, Galbo H. Effect of etanercept in polymyalgia rheumatica: a randomized controlled trial. Arthritis ResTthe 2010;12(5):R176./span/p p dir="ltr"span style="font-size:11px;"10.nbsp;nbsp; nbsp;Salvarani C, Macchioni P, Manzini C, et al. Infliximab plus prednisone or placebo plus prednisone for the initial treatment of polymyalgia rheumatica: a randomized trial. AnnInter Med 2007;146(9):631-639./span/p divnbsp;/div /div












If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.