Blogs
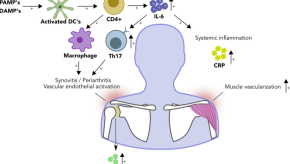
What Goes Wrong with the Immune System in PMR?
Polymyalgia rheumatica (PMR) is a common inflammatory rheumatic disease. The exact trigger for PMR onset remains unknown. However, immunology studies and clinical trials with biological DMARDs now shed light on the immune pathways involved in PMR.Using Methotrexate in PMR
Treatment of PMR is still largely based on glucocorticoids. Where in other inflammatory rheumatic disorders, such as RA and PsA, early initiation of methotrexate is common practice, this is not the case in PMR.Frailty in PMR: Why do I need to care?
It is important to clarify that frailty is not a synonym of age (chronological age). Although there are only a few studies studying the impact of frailty in PMR, frailty is a relevant issue due to several important factors.IL-6 Inhibitors in PMR: Give early or late?
It's exciting to be able to have this conversation because it's only in the past year that we have an approved non-corticosteroid therapy for PMR that's been shown to be effective in a well done clinical trial.PMR: glad or bad tidings?
Please don’t tell your patient that PMR “typically” lasts two years. According to real-world data from the UK, one in four patients with PMR is prescribed steroids by their primary care physician for over four years. But nobody tells them this at the start, and that causes big problems later on.Steroid Tapering in PMR: What's the Gold Standard?
Today I will be talking about the gold standard tapering of glucocorticoids and polymyalgia rheumatica or PMR. Now, whenever we talk about a gold standard, it gets tricky because in practice, so many factors influence the way that we approach glucocorticoids and tapering in PMR.