Blogs
Methotrexate in PsA
Until the publication of the SEAM trial, evidence in the medical literature for the efficacy of the most commonly used drug for psoriatic arthritis worldwide, methotrexate, has been lukewarm at best. Yet we all employ it commonly, either as monotherapy or in combination with biologic or targeted synthetic DMARD treatment. It is inexpensive and widely available, and only modestly toxic.Combined Clinics for PsA
Recognizing the importance of addressing all aspects of disease, we started our joint rheum-derm psoriatic disease clinic at Northwestern shortly after I arrived at the institution, and it has been a tremendous success.MDA: Aiming for Perfection in PsA
When it comes to psoriatic arthritis clinical trials such as TICOPA (tight control in PsA) have consistently shown that treating to target correlates with improved disease domain and patient reported outcomes. Minimal disease activity (MDA) has become an oft used target and outcome in PsA trials. While many of us measure and record a variety of measures in our patient charts, we may be on our way to demonstrating MDA in practice. Here is a quick review of MDA components and how to capture them for your patients.The Enthesitis Challenge in Psoriatic Arthritis
A colleague of mine once told me an interesting story of how her father, who was a doctor, misdiagnosed his wife with fibromyalgia when she actually had psoriatic arthritis with enthesitis all along. I would venture out and say that the average physician would have trouble evaluating enthesitis because even we, as rheumatologists do!Combination Biologic Therapy in PsA: The beginning of a new era?
Without question, basic immunology is at the foundation of rheumatology as a discipline. Indeed, for many rheumatologists, it was the intricacies of the immune system that attracted us into the field. With each passing year, extraordinary advances in scientific methods begat tremendous gains in our understanding of the immune system. Excitingly, we may be entering a new era, driven by results in psoriatic arthritis and other related diseases.Best of 2021: Drug Safety Risk Communication- The 800 lb Gorilla Approach
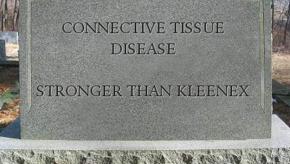
Discussions on drug safety can be as treacherous as quicksand for the patient and physician. What the physician knows and what the patient perceives may not be in sync.
ICYMI: Drug Safety Risk Communication- The 800 lb Gorilla Approach
Discussions on drug safety can be as treacherous as quicksand for the patient and physician. What the physician knows and what the patient perceives may not be in sync.