Can Rituximab Change the Course of Interstitial Lung Disease? Save
Like other extraarticular manifestations, rheumatoid (RA) or connective tissue disease (CTD) related interstitial lung disease (ILD) is difficult to identify early and equally challenging to treat.
Some of our best biologic (TNF inhibitors) or DMARD agents (MTX) have not proven effective in treating ILD.
There have been antecdotal reports of some success using the B cell monoclonal antibody rituximab for such patients. Sharp and colleagues from North Bristol have reviewed their experience with managing patients with CTD-associated ILD with rituximab (RTX) and reported this in the April issue of Rheumatology.
Twenty-four patients were identified who had been treated with rituximab. Their diagnoses included dermatomyositis (3), anti-synthetase syndrome (10), scleroderma (3), SLE (2), Sjogrens (2) and 4 with unclassifiable CTD-ILD. Prior to RTX, 16 received IV cylophosphamide, 9 mycophenolate and 16 IV methylprednisolone.
The response to these therapies (pre-RTX) wa disappointing, with a mean change in forced vital capacity (FVC) prior to therapy of - 3.3% and mean change in diffusing capacity of carbon monoxide of - 4.3%.
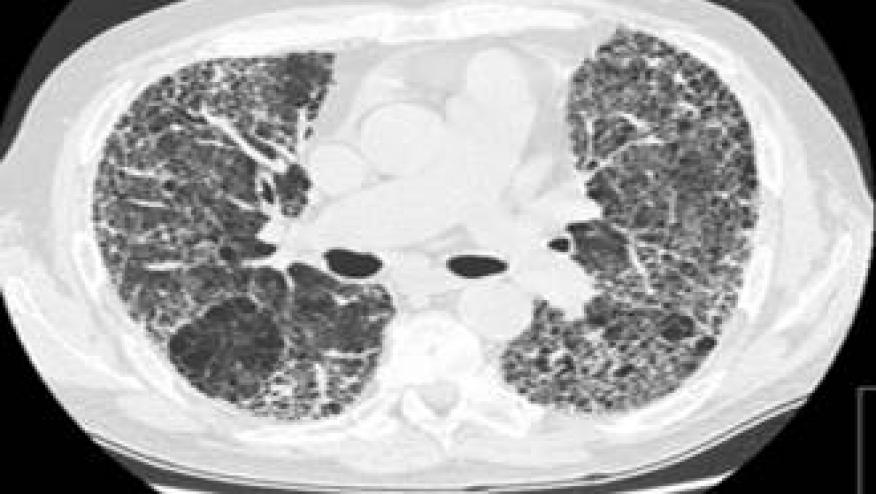
After rituximab, and with a mean followup of nearly 30 months, ILD imaging (HRCT) remained stable or improved for 11 patients, while worsening was observed in 9 patients. The decline in FVC was halted following treatment, with a mean change of + 4.1% (95% CI 0.9, 7.2), while diffusing capacity of carbon monoxide was stable [mean change +2.1% (95% CI - 1.0, 5.2)]. Patients with myositis overlap or antisynthetase syndrome appeared to respond well to treatment, with four patients showing clinically significant improvement in FVC >10%.
Variable responses to RTX treatment may reflect the heterogeneity of the patients studied and the observational nature of this retrospective analysis.
Nevertheless, these data suggest a potential role for RTX, expecially in patients with myositis overlap or antisynthetase syndrome.






If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.