Changing my Mind at EULAR Save
Each year I attend I hope that I’m going to come across something that changes my practice and this year, I think I may have struck gold at a session on Giant Cell arteritis at EULAR in Amsterdam.
It was, as all the best sessions are, based around case presentations of challenging cases and discussions of the management of those cases by experts in the area. Some of the best stuff comes through live conversations with experts where they drop their guard and let you know what they REALLY think.
This session consisted case histories of 3 GCA patients, followed by state of the art presentations and conversations with two well know experts in the area, Dr Carlo Salvarini and Dr. John Stone . One case presentation described the expert management of a patient with GCA who developed a CVA due to intra-cerebral vascular disease and widespread large vessel involvement while on corticosteroids. Two other cases were presented which highlighted the complications of corticosteroid therapy and the dramatic steroid sparing potential of tocilizumab (TCZ).
The ‘elephant in the room’, according to John Stone are corticosteroids, the side effects they cause, and how poor existing treatments are at allowing us to wean our patients off them (only 33% of our GCA patients will be in remission at the end of 1 year). In support of the use of TCZ, Stone highlighted the results of the GiACTA trial (the phase III randomised controlled trial evaluating the efficacy of TCZ in GCA); patients treated with TCZ were much more likely to achieve steroid free remission at 52 weeks (56%) compared to those in the placebo arm of the study (18%). Patients taking TCZ also required approximately 50% less steroids.
Whats not to like? One potential problem highlighted by Stone was the fact that the ESR and CRP may not be helpful (and even misleading) in helping identify patients with flare ups in TCZ treated patients and the fact that up to 25% of patients may not respond at all to the drug.
What was most interesting to me however, based on the relaxed Q+A session that followed the formal talks, was that neither expert, when pressed would even consider treating their patients with more traditionally used ‘steroid sparing agents’ such as methotrexate or azathioprine. They cited poor evidence for efficacy of both drugs. Don’t waste your time prescribing drugs that don’t work, use TCZ, and use it early seemed to the combined take home message from both experts. I was sold and left the session converted.
Until later on that day.
I was speaking to a rheumatology colleague (a vasculitis boffin) over a beer (and with the evangelical enthusiasm of the recently converted), expounding on the benefits of TCZ in GCA and relaying what had been discussed at the session. But he was sceptical.
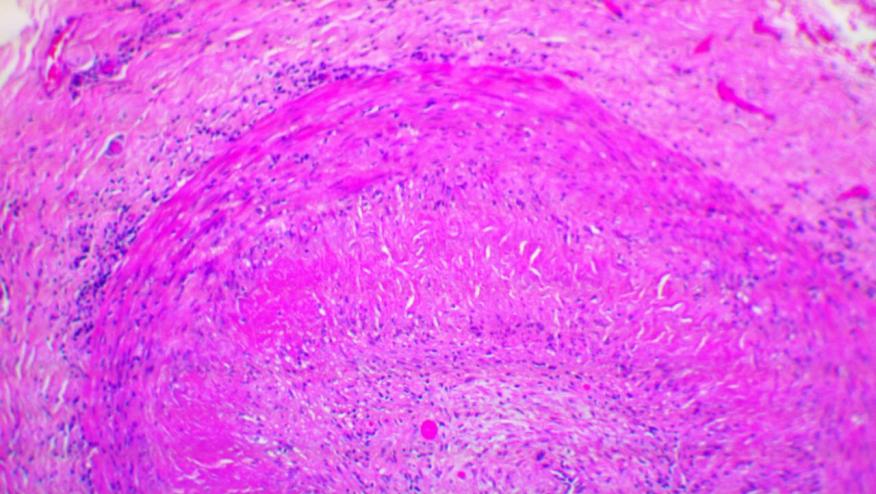
“I don’t use it at all” (TCZ). His concern (and this was alluded to briefly at the session) is that whereas TCZ appears very effective at suppressing systemic inflammation (which is why patients feel so much better on treatment), it may not be as effective at treating the vascular component of GCA.
Work done by Connie Weyand, he explained (while sipping his beer), suggests that IL6 blockade may be effective at suppressing TH17 responses but not Th1 responses. This might put patients treated (apparently successfully) with TCZ at risk of vascular complications. To illustrate his point, he described a patient he had treated with TCZ as a steroid sparing agent who developed large vessel disease (despite a normal ESR and CRP) and an RA patient who had developed new onset GCA despite treatment with TCZ. But like Stone and Salvarini he doesn’t appear to have much faith in methotrexate or azathioprine either. So whats his go to steroid sparing drug in GCA?
Ustekinumab. Apparently as it suppresses both TH17 and AND TH2 responses. At least it does in mice….
Watch this space.










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.