IL-6 Blocker Succeeds in Real-World Vasculitis Save
Tocilizumab (Actemra) was effective for refractory giant cell arteritis (GCA) in real-world practice, although serious infections occurred relatively frequently, Spanish investigators reported.
Among a cohort of 134 patients treated in an open-label study, clinical improvements were seen in 93.9% after 1 month of treatment, according to Miguel A. González-Gay, MD, PhD, of Hospital Universitario Marqués de Valdecilla in Santander, and colleagues.
However, serious infections developed at a rate of 10.6/100 patient-years but were most common among patients receiving high doses of prednisone, the researchers reported online in Seminars in Arthritis & Rheumatism.
Conventional treatment for GCA, a large-vessel vasculitis that usually afflicts individuals over 50, is glucocorticoids, but adverse effects are common and relapses occur frequently following prednisone taper. The aorta and its major branches are most often affected, and blindness, stroke, and aneurysms can occur.
The cause of the disease is unknown, but proinflammatory cytokines such as tumor necrosis factor (TNF)-α and interleukin (IL)-6 have been implicated.
Multiple immunosuppressive agents as well as TNF inhibitors have been tried, but have shown little or no efficacy. However, two recent clinical trials reported beneficial results with tocilizumab and led to approval of this IL-6 receptor inhibitor for GCA in Europe and the U.S.
But in those trials, as is typical for randomized studies, many patients with comorbidities were excluded, patients with recent-onset disease were included, and follow-up was relatively brief.
Therefore, to evaluate the treatment in a real-life setting that included patients with refractory disease and comorbidities -- the patient population most likely to receive this treatment -- the investigators conducted an observational, retrospective study that included patients from 40 referral centers. All had previously received high-dose prednisone and almost three-quarters had also been given conventional or biologic immunosuppressives such as cyclophosphamide, hydroxychloroquine, abatacept (Orencia), infliximab (Remicade), or rituximab (Rituxan).
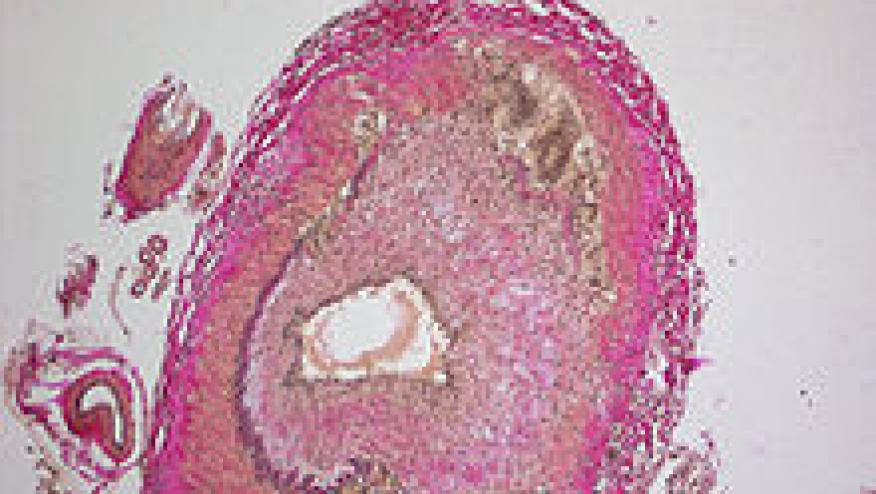
The diagnosis of GCA was confirmed with a positive biopsy of the temporal artery or using imaging techniques such as F-fluorodeoxyglucose PET scanning, MRI angiography, or CT angiography. For acute phase reactants, serum C-reactive protein (CRP) levels above 0.5 mg/dL and erythrocyte sedimentation rates (ESR) above 20 mm/hour in men and 25 mm/hour in women were considered abnormal.
Tocilizumab was given either intravenously, in dosages of 8 mg/kg every 4 weeks, or subcutaneously in a dosage of 162 mg/week, generally with background prednisone (40 to 60 mg/day), which was tapered gradually.
The study included 101 women and 33 men whose mean age was 73. Median disease duration was 13.5 months, and symptoms included headaches, constitutional symptoms such as anorexia and weight loss, jaw claudication, and visual abnormalities.
At month 1, median levels of CRP had declined from 1.7 to 0.11 mg/dL, ESR had fallen from 33 to 6 mm/hour, the percentage of patients with anemia had decreased from 16.4% to 3.8%, and mean hemoglobin levels had risen from 12.3 to 13.1 g/dL (P<0.0001 for all).
In addition, the median dosage of prednisone had already decreased from 15 to 13.75 mg/day (P<0.0001).
Clinical and laboratory improvements persisted throughout follow-up, which extended for up to 4 years, and among those followed for at least 2 years, persistent remission was seen in 39 patients (69.2%), with normal acute phase reactants and prednisone doses ranging from 0 to 5 mg/day.
Of those 39 patients, seven had mild relapses that were treated with small increases in the dose of prednisone.
After a median 12 months of follow-up, 32 patients (23.9%) reported an adverse event, with 17 necessitating discontinuation of treatment. The serious infection rate of 10.6/100 patient-years was higher than the 4.7/100 patient-years seen in a study of patients with rheumatoid arthritis treated with tocilizumab, González-Gay and co-authors noted.
Patients who had serious infections were somewhat older and had longer disease duration. Among patients receiving more than 15 mg/day of prednisone, the rate of serious infections was 16.3/100 patient-years compared with 4.2/100 patient-years among those with dosages below 15 mg/day.
"Taken together, our findings and the results of the randomized controlled trials [suggest that] tocilizumab seems to be an excellent therapeutic option in GCA" and "improves clinical manifestations, acute phase reactants, and imaging findings."
Limitations of the study, the researchers said, included its retrospective and observational design.
The authors reported financial relationships with AbbVie, Merck Sharp & Dohme, Roche, Pfizer, Eli Lilly, Sanofi, Bristol-Myers Squibb, and Janssen.








If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.