Increasing Prevalence and Consequences of Interstitial Lung Disease in RA Save
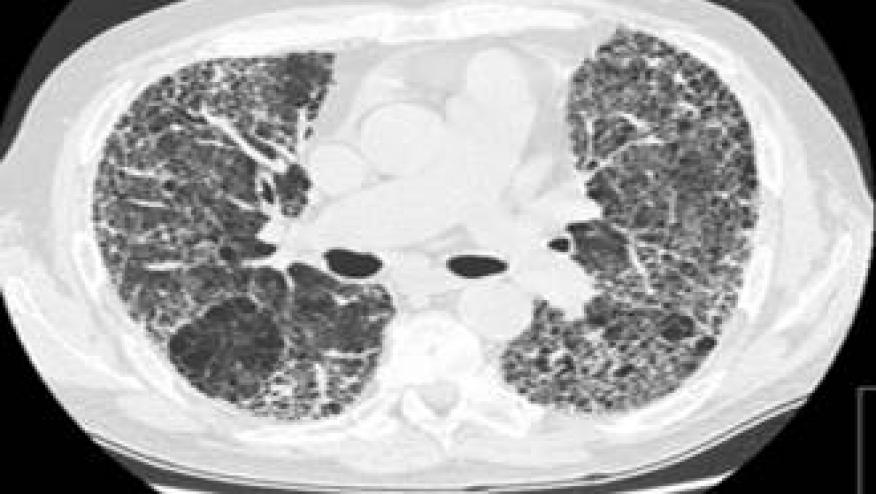
Interstitial lung disease (ILD) has been a hot topic in numerous journals recently with reports of increasing incidence and links to disease activity.
ILD is commonly seen with rheumatoid arthritis (RA) and impart significant morbidity and mortality. The Journal of Rheumatology has reported on the prevalence, incidence, healthcare costs, and mortality of RA-related ILD (RA-ILD) in the United States using claims data from both commercial and Medicare health insurance databases (2003 to 2014).
They found that the prevalence of RA-ILD ranged from 3.2 to 6.0 cases per 100,000 people over a 10-year period and that the prevalence of RA-ILD increased over time.
Analysis of 750 incident patients with 5 years of followup found that 72% had an inpatient admission and 76% had an emergency room visit. Mean total 5-year costs were $173,405 per patient (SD $158,837).
The mortality rate for RA-ILD at 5 years was 35.9%.
Sparks and colleagues also examined ILD, specifically looking at whether disease activity augmented the risk of RA-ILD. (Citation source: https://buff.ly/2YVCPuq)
Using a prospective cohort study with patients from the Brigham RA Sequential Study (BRASS, 2003-2016), they correlated disease activity scores (DAS28) with imaging and pulmonary outcomes. In 1,419 RA patients, they identified 85 incident RA-ILD cases during mean 8.9 years follow-up.
The risk of RA-ILD was increased in patients with moderate or high disease (HR of 2.22; 95%CI 1.28-3.82) compared to those in remission or low disease activity.
Risk for RA-ILD increased with increasing disease activity such that for every unit increase in DAS28, RA-ILD risk increased by 35% (95%CI 14-60%). Results were similar after adjusting for methotrexate, glucocorticoids, bone erosions, or rheumatoid nodules.
England et al analyzed the prospective Veterans Affairs Rheumatoid Arthritis (VARA) Registry, to identify those with chronic lung diseases (CLD) and cardiovascular disease (CVD). (Citation source: https://buff.ly/2P5GEc9)
In their large (n = 2053), predominantly male (91%) RA cohort, 554 (27%) had CLD at enrollment.
RA-CLD patients had an increased mortality risk (HR 1.51; 95% CI 1.26-1.81). This was similar to the mortality seen in RA patients with CVD (HR CVD alone 1.62 [1.35-1.94]). The use of either MTX or biologics did not significantly alter these risks.
The authors suggest that management of comorbid lung disease may be a means of improving long-term outcomes in RA.










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.