JAK Inhibitors Stimulate Osteoblasts Save
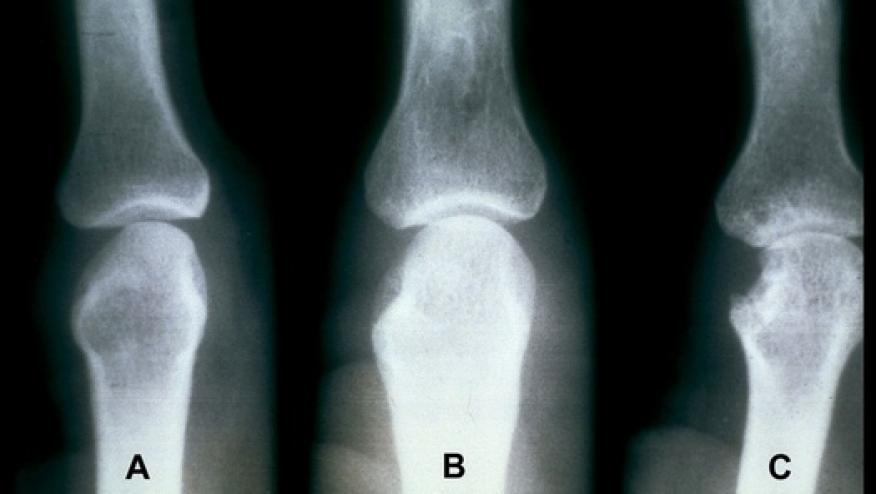
Science Translational Medicine has a report on how the use of Janus kinase (JAK) inhibitors may boost osteoblasts to battle bone erosions in conditions like rheumatoid arthritis (RA).
JAK inhibitors have been shown in clinical trials to retard the development of bone erosions while controlling RA inflammation and other clinical features.
This report reviews how JAK inhibition may influence bone homeostasis using mouse models during steady state or with bone loss induced by estrogen-deficiency or inflammation (arthritis).
In all three situation, JAKi increased bone mass, consistent with reducing the ratio of receptor activator of NF-κB ligand/osteoprotegerin in serum.
Moreover, when tofacitinib and baricitinib were specifically studied, they were shown to significantly increase osteoblast function (P 0.05) without affecting osteoclasts. The JAK inhibitors yielded robust up-regulation of markers for osteoblast function, such as osteocalcin and Wnt signaling and further illustrated by the stabilization of β-catenin.
They postulate that the use of JAK inhibitors in humans with RA may have bone-anabolic effects and further the effort to protect against bony erosions - partly based on their ability to increase osteoblast function and bone formation.










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.