A Link Between Periodontal Disease and Rheumatoid Arthritis Save
Research from Johns Hopkins reports that rheumatoid arthritis (RA) patients with periodontitis exhibited patterns of autoantigen hypercitrullination similar to that seen in RA. Results published in Science Translational Medicine showed that Aggregatibacter actinomycetemcomitans can produce hypercitrullination of patient neutrophils, indicating its possible role in triggering RA. (Citation source: http://buff.ly/2hZTBG8)
These data along with other research pointing the perturbations in the gut microbiome are leading the way to a better understanding of the pathogenesis of RA.
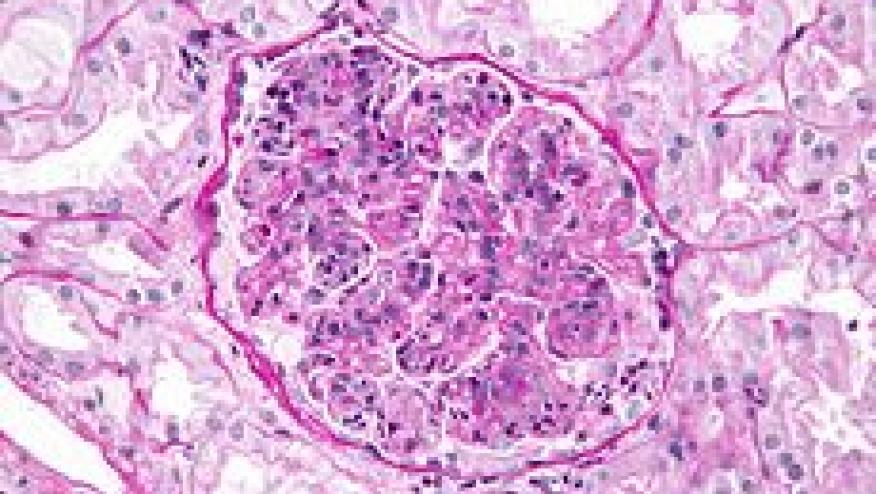
Researchers used mass spectrometry to analyze gingival crevicular fluid (GCF) from patients with periodontal disease and healthy controls. This analysis found that GCF from periodontal disease patients had significantly higher expression of inflammatory markers and was enriched for citrullinated proteins in the periodontal pocket in periodontitis that mirrors the protein citrullination found in the RA joint.
Investigating the mechanisms through which Aa might cause hypercitrullination, the researchers focused on leukotoxin A (LtxA), the organism's major virulence factor, hypothesizing that this factor might dysregulate PAD activation by disrupting neutrophil membranes and allowing an inflow of extracellular calcium. Adding a blocking antibody against leukotoxin A stopped neutrophil hypercitrullination, suggesting that, indeed, LtxA does drive that process.
Proteomic signatures of several microbial species were detected in hypercitrullinated periodontitis samples, including Aggregatibacter actinomycetemcomitans (Aa), but not other candidate pathogens, induced hypercitrullination in host neutrophils.
They also identified the pore-forming toxin leukotoxin A (LtxA) as the molecular mechanism by which Aa triggers dysregulated activation of citrullinating enzymes in neutrophils, mimicking the same pathways that sustain autoantigen citrullination in the RA joint. Moreover, LtxA induced changes in neutrophils mimicks extracellular trap formation, thereby releasing the hypercitrullinated cargo. Exposure to leukotoxic Aa strains was confirmed in patients with RA and was associated with both anticitrullinated protein antibodies and rheumatoid factor.
Ellucidation of these mechanisms opens the door for either new therapeutic interventions or novel ways of monitoring citrullination in RA patients or those at risk.










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.