MMWR: Arthritis Prevalence Increases and Varies Widely Save

MMWR reports that In 2015, the number of adults with arthritis continued to increase; with marked geographic variability in arthritis estimates with gaps in arthritis management.
The CDC estimates that physician-diagnosed arthritis affects 54 million of adults in the United States with an annual cost of approximately $300 billion annually.
The current report used the Behavioral Risk Factor Surveillance System (BRFSS) telephone survey of adults ≥18 years in the United States to assess the age-standardized prevalences of arthritis, arthritis health-related characteristics, and means of arthritis management.
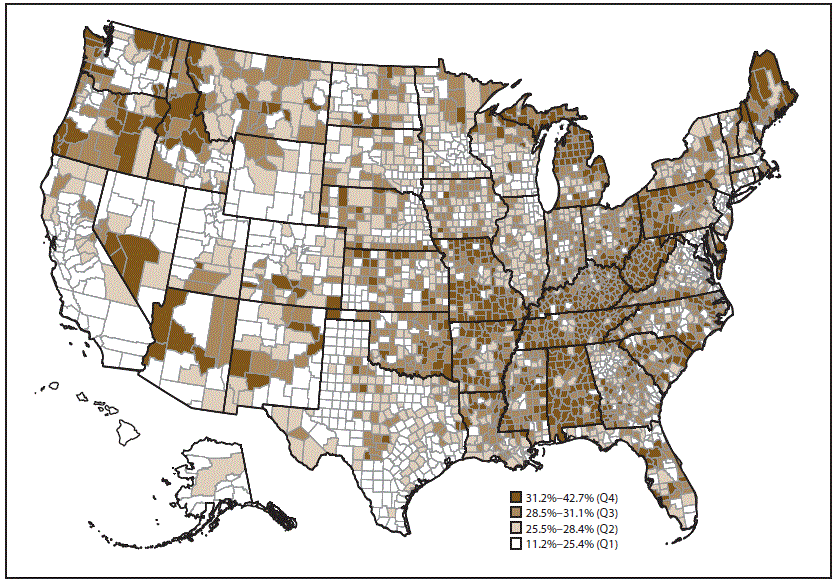
The prevalence of arthritis was 23.0% (range: 17.2%–33.6%); with significant variability by county (range: 11.2%–42.7%).
Arthritis prevalence ranged from a low of 17.2% in Hawaii to a high of 33.6% in West Virginia. At the county level, counties in Appalachia and along the lower Mississippi River tended to have higher predicted prevalences of arthritis. The majority of counties in Alabama, Arkansas, Kentucky, Michigan, Missouri, Tennessee, and West Virginia were in the highest quartile (31.2%–42.7%).
Prevalence* of arthritis among adults aged ≥18 years, by county — Behavioral Risk Factor Surveillance System, 2015
- The prevalence of arthritis among adults with obesity was 30.9% (range: 24.6% in Texas to 41.2% in West Virginia).
- The prevalence of arthritis among adults with coronary heart disease was 44.5% (range: 25.6% in DC to 72.6% in Iowa).
- The prevalence of arthritis among adults with diabetes was 37.3% (range: 27.1% in California to 53.7% in Maine).
Only 13 states have an arthritis management module. Participation in a self-management education course for arthritis was 14.5% (range: 9–19%). Far more were insstructed by a a health care provider to engage in physical activity or exercise (58.5%; range: 52.3%–61.9%), and 44.5% (range: 35.1%–53.2%). were told to lose weight (if overweight or obese).
States with the highest prevalence of arthritis had the highest percentages of arthritis-related health consequences, such as characteristic activity limitations, severe joint pain, and arthritis-attributable social participation restriction, and the lowest percentage of leisure-time walking.
The prevalence of arthritis its management varied across the United States and presents variable challenges in health care delivery at the state and county level.










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.