Nailfold Capillaroscopy Excludes Scleroderma in Raynaud’s Save
The absence of a systemic sclerosis (SSc) nailfold pattern in patients with Raynaud's phenomenon or suspected connective tissue disease is of high clinical value as a biomarker to rule out SSc, according to a large cohort study from the U.K.
For identifying patients who met the 2013 American College of Rheumatology/European League Against Rheumatism or the Very Early Diagnosis of Systemic Sclerosis (VEDOSS) criteria for SSc, the study found that a nailfold capillaroscopy pattern had a negative predictive value of 90% (95% CI 86 to 93), according to Maya H. Buch, MBChB, PhD, and colleagues from the University of Leeds, writing in BMC Musculoskeletal Disorders.
That pattern also had a sensitivity of 71% (95% CI 61 to 80), a specificity of 95% (95% CI 91 to 97), and a positive predictive value of 84% (95% CI 74 to 91).
"We were very impressed with nailfold capillaroscopy's utility in negative prediction," Buch said in an interview with MedPage Today. "The most valuable result here is the low likelihood of scleroderma in patients with Raynaud's phenomenon who do not have any scleroderma-specific features on nailfold capillaroscopy. In practice, this means we can more confidently reassure such a patient and discharge care back to the patient's general practitioner."
The researchers noted that to the best of their knowledge, this is the first study to demonstrate that the absence of any SSc pattern on nailfold capillaroscopy maintains its known negative predictive value, including for patients with secondary Raynaud's phenomenon, who are considered at increased risk of SSc. "This study is only one of two to include a large unselected cohort of patients with Raynaud's phenomenon -- mirroring clinical practice in which rheumatology departments frequently receive referrals of patients with Raynaud's from GPs," Buch said.
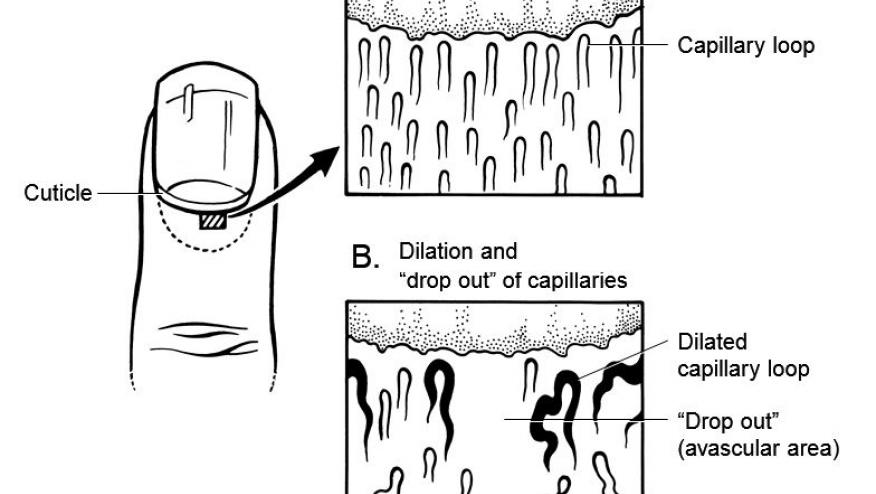
Primary Raynaud's phenomenon is associated with normal microcirculation architecture, whereas microangiopathies are associated with secondary Raynaud's, she explained. The SSc nailfold capillaroscopy pattern correlates with disease duration and severity, and also predicts future vascular and visceral organ damage. Nailfold capillaroscopy also detects vascular problems in glaucoma.
Although an SSc nailfold capillaroscopy pattern is sometimes present in other connective tissue diseases, "nailfold capillaroscopy could be performed to provide reassurance to the rheumatologist in the assessment of both [primary and secondary] Raynaud's phenomenon," the researchers wrote.
Buch and colleagues studied 347 patients referred for nailfold capillaroscopy to a tertiary-care center from January 2009 to October 2013. The mean age of the cohort was 47 years and 83% were female. Clinical review showed that 54 patients (16%) did not have true Raynaud's phenomenon, 69 (20%) had primary Raynaud's, 172 (50%) had secondary Raynaud's, and 52 (15%) had SSc.
At referral, 46 patients (89%) met either VEDOSS or the 2013 American College of Rheumatology/European League Against Rheumatism (ACR/EULAR) criteria for SSc. Of the patients with secondary Raynaud's, 71 (41%) were being managed for connective tissue disease or inflammatory arthritis, while 101 (59%) had an antibody and/or a red-flag feature for SSc.
A nailfold capillaroscopy pattern for SSc was detected in 80 patients (23%) -- 43 with early, 31 with active, and six with late-pattern vasculopathy. This pattern was observed in 37 patients (71%) diagnosed with SSc, 30 (17%) with secondary Raynaud's, nine (13%) with primary Raynaud's, and four (7%) without Raynaud's.
Considering only those patients with non-SSc connective tissue disease or inflammatory arthritis, 16 of 71 patients (23%) had an SSc pattern. This was detected in two of five patients with SLE, eight of 42 with undifferentiated connective tissue disease, four of six with mixed connective tissue disease, one of three with Sjogren's syndrome, and one of 14 with inflammatory arthritis.
Interestingly, the team said, participants meeting ACR/EULAR criteria were more likely to have an SSc nailfold capillaroscopy pattern than those meeting the VEDOSS criteria were: 84% versus 42%, respectively. "This may be related to the earlier stage of disease in those meeting VEDOSS with less time for detectable vasculopathic changes at the nailfold to develop," the researchers wrote. "These findings are important as the earlier detection and management of SSc may lead to reduced morbidity and earlier detection of its complications."
Among the study limitations were the lack of formal measurements to determine enlarged capillaries and the use of two different nailfold capillaroscopy methods, which might have introduced bias. As in clinical practice, the examiners were not blinded to the clinical diagnosis, possibly introducing investigator bias. In addition, the retrospective analysis may have missed important data, particularly the presence of telangiectasia.
The authors cited the need for larger, more defined prospective studies of a heterogeneous group of Raynaud's patients. Buch noted that the current study is part of a larger Leeds program to identify biomarkers for accurately identifying patients at risk for scleroderma or those with scleroderma at risk for poorer outcomes.
The research was supported by the ACORN charity. The authors reported having no relationships with industry.
This article is brought to RheumNow readers by our friends at MedPage Today, where it was originally published on August 25, 2016.










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.