NEJM Review - Glucocorticoid-Induced Osteoporosis Save
Lenore Buckley and Mary Humphrey have published a nice review of glucocorticoid-induced osteoporosis (GIOP) in the NEJM.
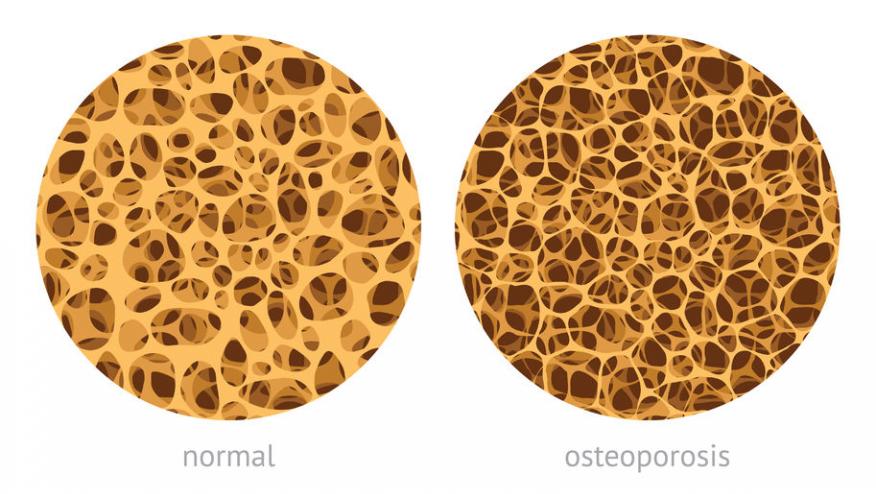
GIOP is a common problem and the consequences can be catastrophic, especially in an aging population and patients with rheumatic disease. This review highlights those at risk, the consequences, treatments (including calcium, vitamin D, bisphosphonates, anabolic and biologic therapies), guidelines and recommendations.
Key takeaways include:
- Risk factors for glucocorticoid-induced fractures include age (>55 years), female sex, white race, and long-term use of prednisone at a dose of more than 7.5 mg per day.
- Screening for fracture risk should be performed soon after the initiation of glucocorticoid treatment. The risk of fracture among patients who are 40 years of age or older can be estimated with the use of bone mineral density testing and the fracture risk assessment tool (FRAX).
- Patients who receive glucocorticoids should be counseled about adequate intake of calcium and vitamin D, weight-bearing exercise, and avoidance of smoking and excessive alcohol intake.
- Pharmacologic treatment is strongly recommended for anyone who has had a fracture and for patients who are at least 40 years of age if, according to the FRAX tool, the risk of major osteoporotic fracture is 20% or higher or the risk of hip fracture is at least 3%. Among patients who are receiving glucocorticoids and have a bone mineral density T score of −2.5 or less (indicating osteoporosis) at either the spine or the femoral neck, pharmacologic treatment is also recommended for men who are 50 years of age or older and for postmenopausal women.
- Bisphosphonates are recommended as first-line treatment of osteoporosis because of their low cost and safety.
- The risk of fracture decreases rapidly when glucocorticoids are discontinued. Exposure to glucocorticoids should be minimized as much as possible.
The begin with a case: a 75-year-old woman with polymyalgia rheumatica is on prednisone at a dose of 20 mg daily with a plan to taper the dose to 5 mg daily within 6 months and be on drug for 2 years. Her serum 25-hydroxyvitamin D level is 30 ng per milliliter (74 nmol per liter). Her bone mineral density T score is −1.2 at the femoral neck.
How would you advise to prevent glucocorticoid-induced osteoporosis and fracture?










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.