New Classification of Idiopathic Inflammatory Myopathies Save
Using an observational cohort analysis of patients in the French myositis network, researchers have proposed a new classification of idiopathic inflammatory myopathies (IIM) with four subgroups: dermatomyositis, inclusion body myositis, immune-mediated necrotizing myopathy, and antisynthetase syndrome.
Rsearchers set out to define a classification system for IIM based on phenotypic, biological, and immunologic criteria.
The French myositis network includes patients referred for evaluation of neuromuscular diseases. From this database they identified 260 adult patients with myositis who had complete data and defined historical classifications for polymyositis, dermatomyositis, and inclusion body myositis. The dataset included a total of 708 clinical, serological and comorbidity variables (eg, cancer, lung involvement, and myositis-specific antibodies).
All patients were extensively tested tested for anti–histidyl-ARN-t- synthetase (Jo1), anti–threonine-ARN-t-synthetase (PL7), anti–alanine-ARN-t-synthetase (PL12), anti–complex nucleosome remodeling histone deacetylase (Mi2), anti-Ku, anti–polymyositis/systemic scleroderma (PMScl), anti–topoisomerase 1 (Scl70), and anti–signal recognition particle (SRP) antibodies.
Two-thirds of this population were women with a mean age of 60 years. Analysis revealed 4 patient clusters:
- Inclusion body myositis (n = 77) - included patients who were male, white, and older than 60 years and had finger flexor and quadriceps weakness and findings of vacuolated fibers and mitochondrial abnormalities. Cluster 1 regrouped patients who had inclusion body myositis (72 of 77 patients [93.5%]; 95% CI, 85.5%-97.8%; P < .001).
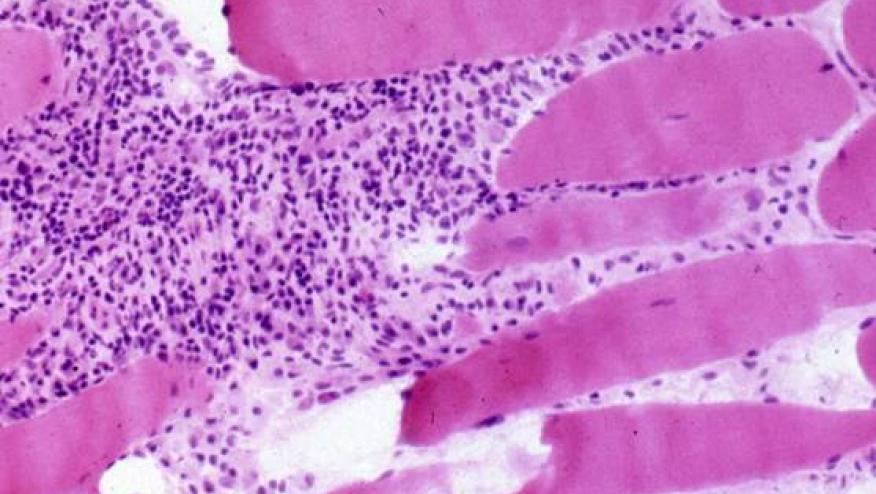
- Immune-mediated necrotizing myopathy (n = 91) regrouped patients who were women and had high creatine phosphokinase levels, necrosis without inflammation, and anti–SRP or anti–3-hydroxy-3-methylglutaryl-coenzyme A reductase (HMGCR) antibodies corresponding to immune-mediated necrotizing myopathy (53 of 91 [58.2%]; 95% CI, 47.4%-68.5%; P < .001).
- Dermatomyositis (n = 52) regrouped patients who had dermatomyositis rash and anti-Mi2, anti–melanoma differentiation-associated protein 5 (MDA5), or anti–transcription intermediary factor-1γ (TIF1γ) antibodies, mainly corresponding with patients who had dermatomyositis (43 of 52 [82.7%]; 95% CI, 69.7%-91.8%; P < .001).
- Antisynthetase syndrome (n = 40) was defined by the presence of anti-Jo1 or anti-PL7 antibodies corresponding to antisynthetase syndrome (36 of 40 [90.0%]; 95% CI, 76.3%-97.2%; P < .001). The classification of an independent cohort (n = 50) confirmed the 4 clusters (Cohen κ light, 0.8; 95% CI, 0.6-0.9).
These cluster analyses of retrospective database findings suggest that IIM can be classifed into these 4 subgroups, thereby facilitating better identifications of patient subsets based on a clinical-serologic approach, potentially leading to earlier diagnoses and more efficient future therapies.










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.