New EMA Warnings for Tofacitinib in Patients at Risk for Clots Save
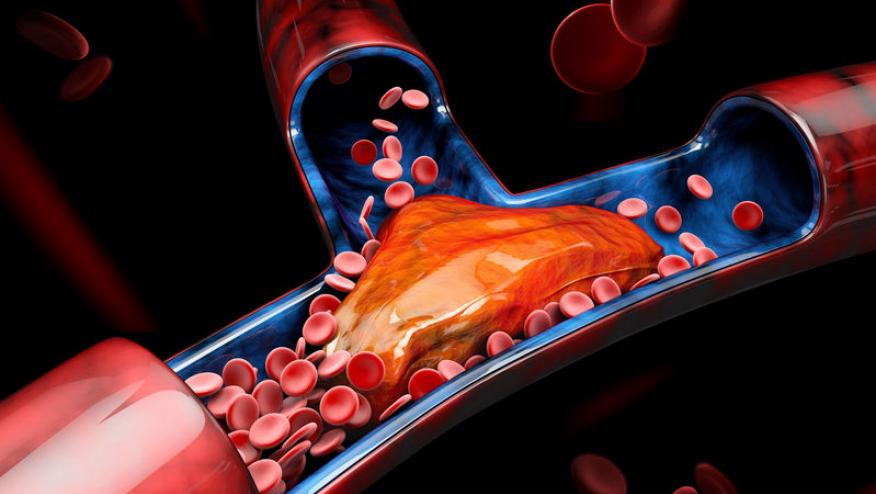
The European Medicines Agency (EMA) safety committee (PRAC) has concluded that Xeljanz (tofacitinib - TOFA) could increase the risk of blood clots in the lungs and in deep veins in patients who are already at high risk for venous thromboembolic events (VTE). The PRAC is recommending that TOFA should be used with caution in patients at high risk of blood clots (VTE), regardless of dose used.
As was previously concluded by the EMA and FDA, the use of TOFA at high doses (10 mg twice daily) should not be used in rheumatoid arthritis as Pfizer's long-term safety study has shown significant risk of VTE and death (compared to RA patients treated with adalimumab. This higher dose was previouly approved only for use in ulcerative colitis (by EMA and FDA). But now the EMA PRAC is advising that the 10 mg bid dose should not be used in ulcerative colitis patients who are at high risk unless there is no suitable alternative treatment.
Further, the PRAC is recommending that patients older than 65 years of age should be treated with Xeljanz only when there is no alternative treatment. Patients at high risk of blood clots include those who have had a heart attack or have heart failure, cancer, inherited blood clotting disorders or a history of blood clots, as well as patients who take combined hormonal contraceptives, are receiving hormone replacement therapy, are undergoing major surgery or are immobile.
Doctors should also consider other factors that may increase the risk of blood clots including age, obesity, diabetes, hypertension or smoking.
These recommendations follow the PRAC’s review of an ongoing study (study A3921133) in patients with rheumatoid arthritis and an increased risk of cardiovascular disease. This study showed an increased risk of blood clots in deep veins and in the lungs with both the 5 mg and 10 mg twice daily doses of Xeljanz as compared with patients taking TNF-inhibitors.
The PRAC also re-assessed additional data from earlier studies. All data combined showed that the risk of blood clots was higher in patients taking Xeljanz, especially with the 10 mg twice daily dose and in those being treated for an extended period. Results also showed a further increased risk of serious and fatal infections in patients older than 65 years of age.
The product information for Xeljanz will now be updated with new warnings and recommendations based on data from the study and will list blood clots as an uncommon side effect occurring in between 1 in 1,000 and 1 in 100 patients.
TOFA (Xeljanz) was first authorised in the EU on 22 March 2017 to treat adults with moderate to severe rheumatoid arthritis (a disease that causes inflammation of the joints) at a dose of 5 mg bid or 11 mg once daily. In 2018, its use was extended to treat adults with psoriatic arthritis (red, scaly patches on the skin with inflammation of the joints) and severe ulcerative colitis (a disease causing inflammation and ulcers in the lining of the gut).










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.