Obesity Surgery Tames Knee OA Pain Save
Laparoscopic gastric band (LAGB) surgery was associated with significant decreases in knee pain from osteoarthritis (OA), with the greatest improvements seen among those whose body mass index (BMI) had the greatest decreases and among younger patients, researchers reported.
Among patients whose BMI decreases following bariatric surgery exceeded 13 kg/m2, pain reduction from baseline was 4.23 points on a 0-10 scale, whereas the decrease was only 2.59 points for those whose BMI decline was less than 8 kg/m2, according to Jonathan Samuels, MD, and colleagues from NYU Langone Medical Center in New York City.
And for patients age 40 and under, the pain improvements were 4.41 points compared with 4.11 for those 41 to 50, 3.25 for those 51 to 60, and only 2.11 among those older than 60, the researchers reported in Seminars in Arthritis & Rheumatism.
Osteoarthritis is now the leading cause of musculoskeletal disability in the U.S., and available treatments are insufficiently effective and can be associated with major toxicities.
Obesity is arguably the most modifiable risk factor for knee OA, doubling the lifetime risk for the progressively painful condition. Many organizations, including the American College of Rheumatology and the Osteoarthritis Research Society International, advocate weight loss as a therapeutic strategy for decreasing knee pain.
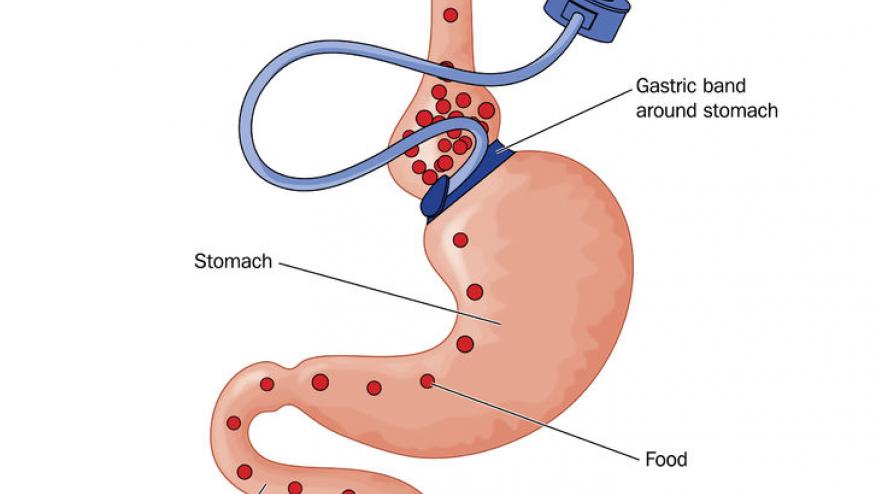
The National Institutes of Health guidelines on bariatric surgery recommend the more aggressive procedures of gastric bypass and sleeve gastrectomy for patients whose BMI is 35 or higher and who have at least one comorbid condition, and also the less invasive LAGB for patients with less severe obesity (BMI of 30 or higher) and one or more comorbidities.
"Yet most insurance companies deny coverage for the LAGB in the 30 to 35 kg/m2 range, despite early evidence that moderately obese patients achieve a significant reduction of knee OA pain following the less aggressive LAGB procedure," Samuels and colleagues wrote.
In order to identify groups of patients who might have the greatest benefits from bariatric surgery and should therefore consider it earlier, before irreparable knee damage occurs, the researchers reviewed the Weight Management Program Research Registry for patients who had one of the bariatric procedures from 2002 to 2015. Eligible patients completed a telephone survey on pain 1 year after the surgery and in the subsequent years.
Of the 120 patients who had the LAGB surgery, mean age was 49.7, and more than three-quarters were white women. The mean baseline BMI was 46.3, and mean knee pain score was 6.88.
One-third of the patients had previously had a knee injury, and one in five had prior knee surgery. A total of 47% had OA in sites other than the knee, and 53% had a family history of OA.
A year after surgery, the mean BMI had declined by 11.2 kg/m2 to an average of 35.1 (P0.00), while knee pain decreased to a mean score of 3.34 (P0.001). Higher baseline BMI did not predict the degree of knee pain reduction, as might have been expected. "Thus, as suggested by the recent guidelines on comorbidities of obesity, LAGB may be a viable treatment method for those with BMI of 30 kg/m2 or higher, even though insurers generally do not reimburse unless the BMI is at least 35 kg/m2," the researchers wrote.
"We thought it would be helpful to show that people with more modest obesity can do really well with the surgery," Samuels told MedPage Today.
The mean time between the surgery and the survey was 9.14 years. By that point, knee pain scores had declined further, to a mean of 2.84 (P=0.054), and mean BMI was 33.8.
Having had a serious knee injury before the development of OA was associated with less of an improvement in pain, with mean changes in pain scores of 2.87, but a prior history of knee surgery showed no association. There also was no difference for sex or family history, and those with OA at multiple sites had less improvement.
"For obese patients who have persistent and severe knee pain from osteoarthritis, weight loss surgery should be considered a treatment option regardless of age," Samuels said.
"Understandably, as older individuals are more likely to have advanced OA, the greater knee pain reduction among younger individuals may have resulted to some extent because they had less severe OA than their older counterparts," the team concluded. "Still, younger patients who are not originally candidates for LAGB should be reconsidered if they also have debilitating knee OA pain."
Limitations of the study, the researchers said, included its retrospective design and the lack of radiographic evidence of knee OA.
The study received no funding.
One co-author reported consulting for Arrow Inc.










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.