Preventing Hep B Reactivation Due to Immunosuppressive Drug Treatments Save
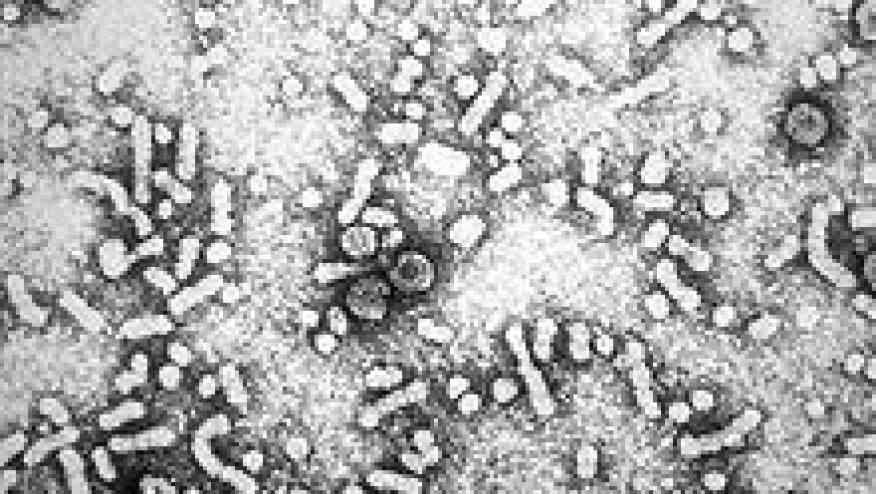
Reactivation of hepatitis B virus infection can have devastating consequences, especially amongst those patients receiving immunosuppressive therapy.
HBV reactivation, with hospitalization or fatal outcomes have been described in patients receiving rituximab, TNF inhibitors (infliximab, etanercept, adalimumab), abatacept, tocilizumab, azathioprine and prednisone to name a few. Interestingly, there have been no or few reports of HBV reactivation in rheumatic patients receiving methotrexate, anakinra or tofacitinib. Importantly, reactivation can occur in patients with RA, Still’s disease, psoriatic disease, colitis and spondylitis, cancer and transplantation patients. Those affected are unified by the certain factors that tip the risk in favor of reactivation. There are ways to identify those at high and low risk for reactivation.
Perrillo et al reviews strategies to prevent HBV reactivation in a recent JAMA article. They state that patients with active HBV infection who are HBsAg positive are at greatest risk for reactivation. HBsAg+ patients who are receiving chemotherapy have a 40% risk of HBV reactivation with a subsequent risk of liver failure (13%) or death (16%).
Patients who have resolved HBV infection (HBsAg negative and HBcAb positive) are at a much lower risk of HBV reactivation. In my review of the literature, reactivation was seen in < 1% of patients on TNF inhibitors with resolved HBV infection. Perillo estimates the risk w/ TNF inhibitors to be 0-5% and 3-41% for patients receiving R-CHOP (with RTX rituximab, cyclophosphamide, hydroxydaunorubicin, oncovin, and prednisone). Hence, the depth of immunosuppression (augmented by cytotoxics, radiation, high dose steroids) may substantially augment the low risk that accompanies a resolved HBV serologic profile.
Current recommendations include:
-
All patients starting immunosuppressive therapy (biologics, DMARDs, high dose steroids, chemotherapy) should be screened for active, resolved/occult HBV (and hepatitis C) infection.
-
Patients who are HBsAg+ should avoid immunosuppressives, but if required, such patients should receive antiviral prophylaxis (e.g., lamivudine, entecavir, tenofovir, etc). Prophylaxis should also be given to selected resolved HBV patients who are HBsAg negative and anti-HBc–positive who will receive B-cell–depleting agents or other highly aggressive chemotherapy. Prophylaxis is not 100% effective and patients should have their hepatic enzymes and HBV DNA levels monitored regularly and continued for up to 12 months after suspension of immunosuppression.










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.