Serious Infections are Increasing in Lupus Save
Tektonidou and coworkers have analyzed hospitalized serious infections (SIE) involving lupus patients over a 15 year period and show that SIE in SLE have increased substantially between 1996 and 2011, and in 2011 are 12 times higher than seen in patients without SLE.
They estimat the number of hospitalized pneumonia in SLE was 4,382 in 1996, followed by sepsis (2,305), skin infections (1,422), UTI 643), and opportunistic infections (370). Rates were much higher in patients with SLE than in those without SLE, with age-adjusted relative risks ranging from 5.7 for pneumonia to 9.8 fold higher for urinary tract infection in 1996. Mortality rates in lupus patients were higher in those with opportunistic infections and those requiring mechanical ventilation.
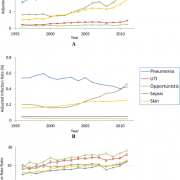
Reasons for this increase over time are not apparent. While it is tempting to ascribe this to increased use of steroids or immunosuppressives, there is no evidence to support this. Instead, it may be that lupus patients are living longer and may therefore have more time to develop more comorbidities that can augment the risk of infectious events.










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.