Sjögren's Syndrome Differs in Minorities Save
Minority groups in the U.S. have differing rates of Sjögren's syndrome (SS) and exhibit distinct clinical patterns of the disease, a large cross-sectional study revealed.
The percentage of American Indians in a SS cohort of 610 patients was much higher than expected, at 25.3%, whereas the percentage of African Americans was lower, at 3.1%, according to Astrid Rasmussen, MD, PhD, of the Oklahoma Medical Research Foundation in Oklahoma City, and colleagues.
In addition, American Indians had higher levels of disease activity and more extraglandular manifestations, whereas African Americans had a symptom pattern associated with subsequent lymphoma development, they reported in Arthritis Care & Research.
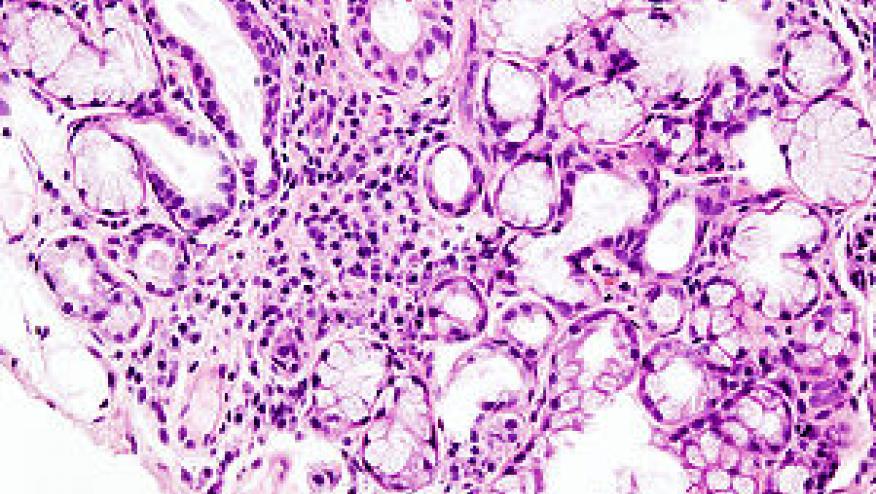
SS is a multifaceted autoimmune disease characterized by dysfunction of the salivary, lacrimal, and other exocrine glands, the presence of autoantibodies, and extraglandular manifestations such as arthritis, lymphadenopathy, vasculitis, and lymphoma. The diagnosis can be difficult because it typically requires multidisciplinary involvement and there is no gold standard test. Therefore, "SS is frequently misdiagnosed, underdiagnosed, or diagnosed at late stages of the disease," the researchers observed.
Moreover, little is known about epidemiology and differences among minority ethnic groups, who often are disproportionately affected by autoimmune diseases.
Accordingly, Rasmussen's group analyzed data from the Oklahoma Sjögren's Syndrome Center of Research Translation, which included almost 1,700 individuals evaluated for sicca symptoms from 2005 to 2017 from the Oklahoma Medical Research Foundation, the University of Minnesota in Minneapolis, Cedars-Sinai Medical Center in Los Angeles, and the Carolinas Medical Center in Charlotte, North Carolina.
Their analysis included 426 patients self-identified as having European heritage, 164 American Indians, and 20 African Americans. (Other groups such as Asians and Hispanics were not included in the analysis because the numbers were too few.)
Whereas the American Indians comprised one-quarter of the SS cohort, their percentage of the overall population was substantially lower in Oklahoma, at 11.9%, and in the U.S. as a whole, at 1.41%. And whereas African Americans represented <5% of the SS cohort, they comprised 7.3% of the Oklahoma population and 12.6% of the overall U.S. population.
Regarding disease characteristics, fewer American-Indian patients exhibited decreased salivary flow (61.4% vs 70.1%) and tear production (44.5% vs 60.3%) compared with patients of European descent. They also had lower rates than the European ancestry group of autoantibodies including anti-Ro/SSA (OR 0.59, 95% CI 0.41-0.85), anti-La/SSB (OR 0.42, 95% CI 0.28-0.62), and rheumatoid factor (OR 0.58, 95% CI 0.39-0.88). African Americans more often had hypergammaglobulinemia than patients with European ancestry (52.6% vs 23.6%) or American Indians (14.6%).
African Americans also more often had elevated erythrocyte sedimentation rates (47.1%) than the European ancestry group (18.4%) or American Indians (23.2%).
For extraglandular manifestations, articular disease was more common in both American Indians (OR 2.26, 95% CI 1.46-3.47) and African Americans (OR 3, 95% CI 1.16-7.66) than the European ancestry group. Glandular involvement such as parotid swelling was more common among American Indians and African Americans than Europeans, and hematologic abnormalities were more frequently seen in African Americans.
"We found marked differences in the susceptibility to SS in the different races; American Indians are affected at a higher rate than expected based on their proportion of the general population, and African Americans are under-represented ... in comparison to the general population," the researchers wrote.
A similar pattern has been seen with rheumatoid arthritis. Among Caucasians, the annual incidence worldwide has been estimated at 0.5% to 1%, but reportedly is as low as 0.1% among rural residents of Africa and as high as 5% in certain American Indian tribes such as the Pima and Chippewa.
Many studies have documented disparities in access to care and socioeconomic status for minority groups and have linked these factors with poorer outcomes. This may have contributed to some of the differences observed in the current study, and although American Indians tend to have lower socioeconomic status than whites, they do have access to Indian Health Services and other specialty care and may more easily obtain referrals.
"Thus, we hypothesize that the observed differences in disease frequency and phenotype are at least in part due to bona fide biological factors (i.e., population-specific genotypes underlying dysregulation of differing pathways), rather than being purely attributable to marginalization and social determinants," Rasmussen and colleagues wrote.
The observation that American Indian patients in this cohort had fewer of the most prominent SS symptoms and clinical clues such as salivary and lacrimal dysfunction and typical autoantibodies may result in a delay or lack of diagnosis and treatment. Thus, a heightened suspicion is needed in this population.
Similarly, the triad of hypergammaglobulinemia, elevated erythrocyte sedimentation rate, and parotid swelling observed among African Americans has been associated with lymphomagenesis, so more intensive surveillance for malignancy is warranted in this group, the researchers concluded.
A study limitation was its cross-sectional design.









If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.