Stroke Increased in Rheumatoid Arthritis Save
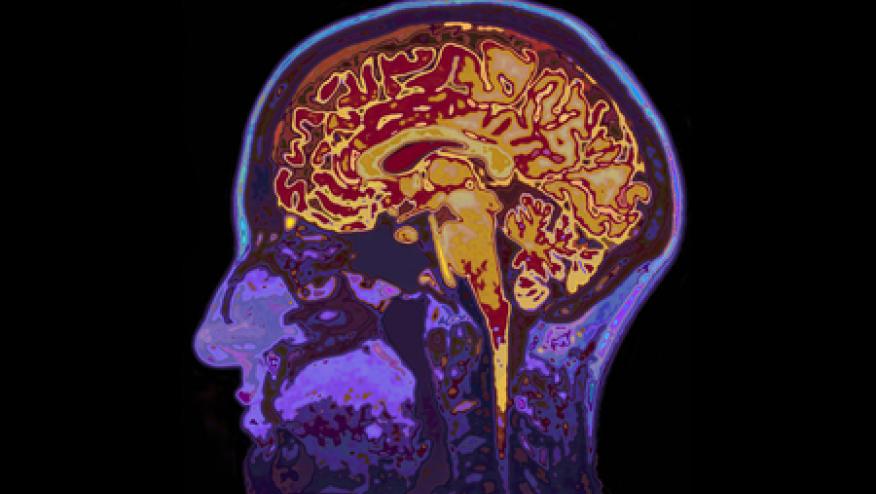
Rheumatoid arthritis (RA) is a chronic, inflammatory disease with systemic effects beyond the joints. While RA patients are known to have signficantly higher risks for cardiovascular disease and venous thromboembolic events, an association with stroke (CVA) is unclear.
A study claims data from Israel analyzed 11,782 RA patients and 57,973 age- and gender-matched controls.
RA patients had more cardiovascular risk factors than controls.
Stroke rates were significantly elevated among young RA patients in comparison with controls (3.74 vs. 2.20%, respectively, p < 0.001).
In multivariate analysis, there was an 18% increased risk of CVA in RA, and RA was found to be independently associated with stroke (OR 1.18, 95% CI 1.09-1.28).
Clinicians should be aware of those factors, in additioni to RA, that may augment the risk of stroke.










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.