Tocilizumab Effective in PMR Save

Polymyalgia rheumatica (PMR) should be easy and responsive, but it can be a challenge and requires long-term steroid therapy. Problems often begin when steroid–induced side effects take their toll on a patient, especially in elderly adults.
To date, clinical trials have failed to identify a reasonable alternative to steroids, with only methotrexate deemed effective. A growing body of case reports and small trials identifies tocilizumab as a potential therapeutic alternative in refractory PMR.
A 24-week, open-label, longitudinal, prospective study of the safety and efficacy of tocilizumab in recent-onset PMR (Tolerance and Efficacy of Tocilizumab in Polymyalgia Rheumatica study) was conducted.
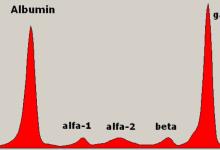
The PMR activity score (PMR-AS) relies on five variables: morning stiffness (in minutes), elevation of the upper limbs (rated 0–3), physician's global assessment and pain intensity on 10-point visual analogue scales (VASs) and C reactive protein (CRP) level in mg/dL; the erythrocyte sedimentation rate (ESR) can replace CRP was assessed. The prespecified primary end point was the proportion of patients whose PMR-AS was ≤10 at week 12.
Of the 20 patients that completed the study, all patients achieved the primary end point of PMR-AS≤10 by week 12. Median PMR-AS was 36.6 (30.4–43.8) at baseline and 4.50 (3.2–6.8) at week 12 (p0.001). At weeks 16, 20 and 24, the prednisone dosage was decreased according to the study protocol. Median PMR-AS improved significantly from weeks 12 to 24 (from 4.50 (3.2–6.8) to 0.95 (0.4–2.0)). No patient required rescue therapy or had a flare during the prednisone phase.
Follow-up was provided 1 year after the end of prednisone therapy. No patient had flares or giant-cell arteritis. One patient experienced a moderate relapse 2 months after prednisone discontinuation; she had received only two tocilizumab infusions, due to an adverse event, and she achieved a second remission after 4 weeks of prednisone therapy, 5 mg/day.
Although the study was not randomized, and cannot be used to justify active implementation of tocilizumab in routine clinical practice, it deserves attention as a proof-of-concept study. It may warrant future evaluation of tocilizumab as a potential steroid sparing agent for PMR.









If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.