Ultrasound Predicts Inflammatory Arthritis in CCP+ Persons Without Synovitis Save
A prospective study of 136 people who were CCP+, but who had no clinical evidence of synovitis, examined what factors may predict future development of inflammatory arthritis.
After a mean of 18 mos, 42% were diagnosed with inflammatory arthritis and 49/57 met ACR/EULAR criteria for the diagnosis of rheumatoid arthritis (RA).
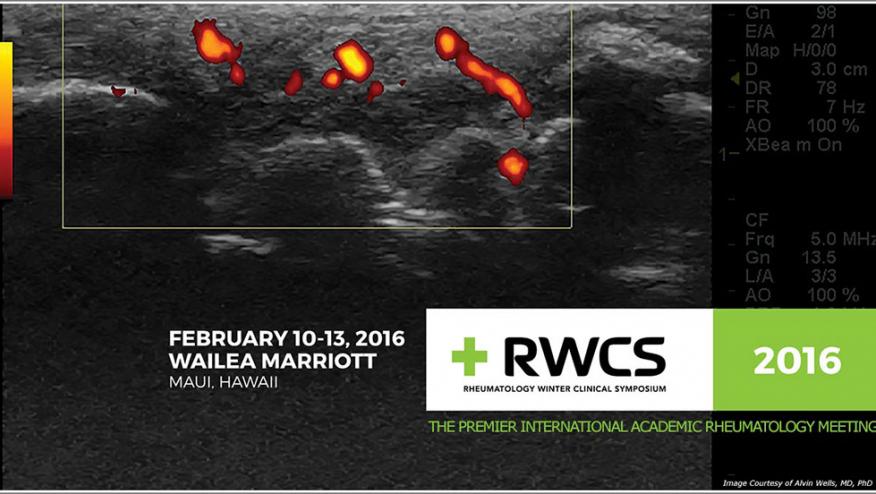
Using ultrasound, 96% of the 136 patients had a gray scale (GS) signal, 30% had a power doppler signal (PD) and 21% had one or more erosions by ultrasound.
Progression to IA was significantly higher in those with ultrasound findings in any joint (excluding MTPs for GS). When ultrasound found a GS ≥2, PD ≥2 or erosion ≥1, a significant 2.3 - 3.7 fold increase risk of future IA was seen.
Ultrasound features of joint inflammation may be detected in anti-CCP-positive patients without CS. Ultrasound findings predict progression (and rate of progression) to IA, with the risk of progression highest in those with PD signal.










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.