Ustekinumab: A Novel Intervention in Giant Cell Arteritis Save
Treatment of refractory giant cell arteritis (GCA) with ustekinumab (Stelara) showed therapeutic promise as a steroid-sparing agent in a small, open-label study, Irish researchers reported.
Among a group of 25 patients who had been unable to taper their corticosteroids without relapsing, the median daily dose of prednisolone decreased from 20 mg/day to 5 mg/day by week 52, according to Richard Conway, MBBCh, PhD, of the Center for Arthritis and Rheumatic Diseases at St. Vincent's University Hospital in Dublin, and colleagues.
"The frequency and severity of glucocorticoid-related adverse events experienced by patients on 15 mg of prednisolone daily is significantly greater than those on 5 mg," the researchers observed. In addition, none of the patients had a relapse while on this treatment, the team reported in Seminars in Arthritis & Rheumatism.
GCA is a systemic vasculitis that can affect any large or medium-sized artery, but most commonly involves the extracranial branches of the carotid, axillary, and subclavian arteries as well as the thoracic aorta. Up to one-quarter of patients develop severe complications including stroke and blindness.
Glucocorticoids are the standard treatment, and often must be given in high doses that are associated with fractures, diabetes, and hypertension. "There remains a critical unmet need for proven safe and effective treatment options to minimize glucocorticoid use and prevent vascular complications in GCA," Conway and colleagues wrote.
Asked for his perspective, Kenneth Warrington, MD, chair of the department of rheumatology at the Mayo Clinic in Rochester, Minn., who was not involved in the study, told MedPage Today, "GCA is a disease where we've had very limited treatment options. We've had steroids since the 1940s, but we only have one biologic recently approved for GCA, tocilizumab [Actemra], so other options are worth exploring."
The rationale for using ustekinumab in GCA lies in earlier observations in a hybrid human/mouse model that two separate pathways are involved in disease pathogenesis, the Th1 pathway and the Th17 pathway, Warrington explained. Acting through these pathways are the cytokines interleukin (IL)-12 and IL-23, both of which are blocked by ustekinumab through binding to the two cytokines' shared p40 subunit, which makes it an "appealing" option, he said. In contrast, steroids work only through the Th17 pathway.
Therefore, to examine the possibility that ustekinumab might be useful in refractory GCA, the investigators undertook a study that included 25 of "our most difficult to treat patients."
Ustekinumab was administered subcutaneously in doses of 90 mg at baseline and week 4 and then every 3 months, with adjustments possible according to the treating clinicians' judgment.
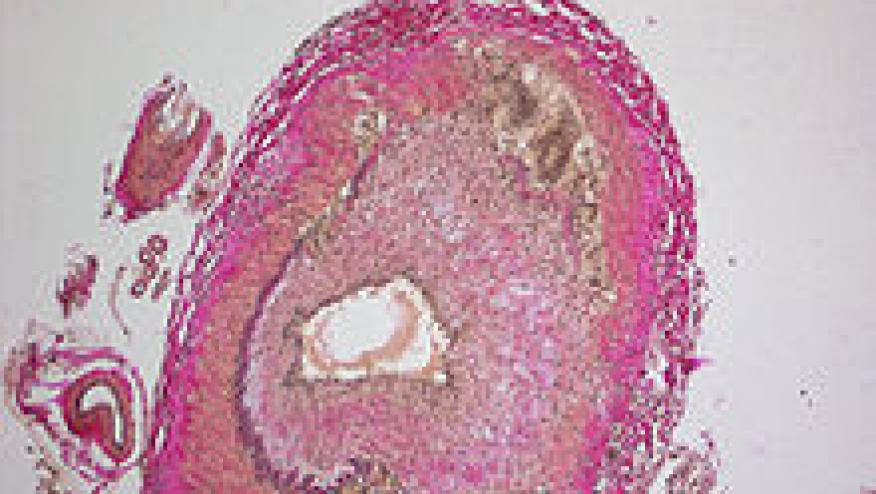
Patients' mean age was 70, and most were women. The median duration of disease was 29 months, and the median number of previous disease relapses was two. Three-quarters of patients had biopsy-proven GCA; the median score on the Vasculitis Damage Index was 1, and the Charlson Comorbidity Index also was 1. Cranial-ischemic complications were present in 20% of patients.
All patients had relapsed on glucocorticoid monotherapy, and 84% had reported significant adverse events to this treatment. Two-thirds had previously received methotrexate in median dosages of 20 mg/week for a median duration of 15 months. Other previous treatments included azathioprine, leflunomide, adalimumab (Humira), and gevokizumab.
At week 24, the median daily dosage of prednisolone had declined from 15 to 7 mg (P<0.001), median erythrocyte sedimentation rate (ESR) had decreased from 29 to 19 mm/h, and median C-reactive protein (CRP) had decreased from 12.9 to 8 mg/L (P=0.011). Three patients had completely discontinued the glucocorticoid, and other immunosuppressants had been stopped in 10 patients.
At week 52, the median cumulative dose of prednisolone since starting ustekinumab was 2,790 mg compared with 5,475 mg in the year before the treatment began. Median ESR had declined to 17 mm/h and CRP was 6 mg/L. Six patients had stopped taking prednisolone and 13 had discontinued their other immunosuppressants.
In six patients, the interval between ustekinumab doses was changed to every 2 months because of persistent symptoms and elevated acute phase reactants, but the glucocorticoid dose was not increased. In four of these, the symptoms resolved and the biomarkers normalized, while in the other two, symptoms persisted but were attributed to other causes such as end-stage renal disease.
Three patients who stopped prednisolone were able to decrease the ustekinumab dosage to 45 mg every 3 months, and responses were maintained. One patient discontinued ustekinumab and was in drug-free remission at 12 months.
In 10 of the patients, CT angiography was performed before ustekinumab treatment was initiated, and on repeat imaging after 10 months no new aneurysms or stenoses were detected and improvement of vessel wall thickening was seen in all.
Eight patients had adverse events, most of which were minor infections, and three patients discontinued therapy.
Limitations of the study, the researchers said, included its single-center design and lack of validated disease activity measures in GCA. In addition, Warrington noted, "this was a small pilot study. It was interesting and encouraging, but requires validation in a placebo-controlled trial."










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.