Anti-Rheumatic Rx

Janet Pope Janetbirdope
1 year 2 months ago
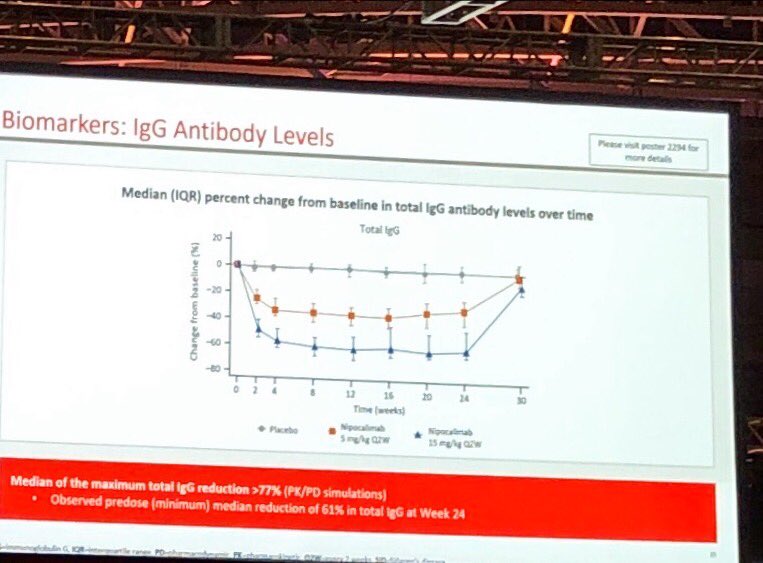
#Positive #RCT of #Nipocalimab a FcRn receptor inhibitor in #Sjogrens #Disease
👏Phase 2 +RCT
ESSSDAI and ESPRI both improved
🤷♀️what it means to lower #antibodoes #Ro #La
Excited for Phase 3 results
#ACRBest #ACR24 @RheumNow @ACRheum abst#2527 https://t.co/NeeYT7VR16

David Liew drdavidliew
1 year 2 months ago
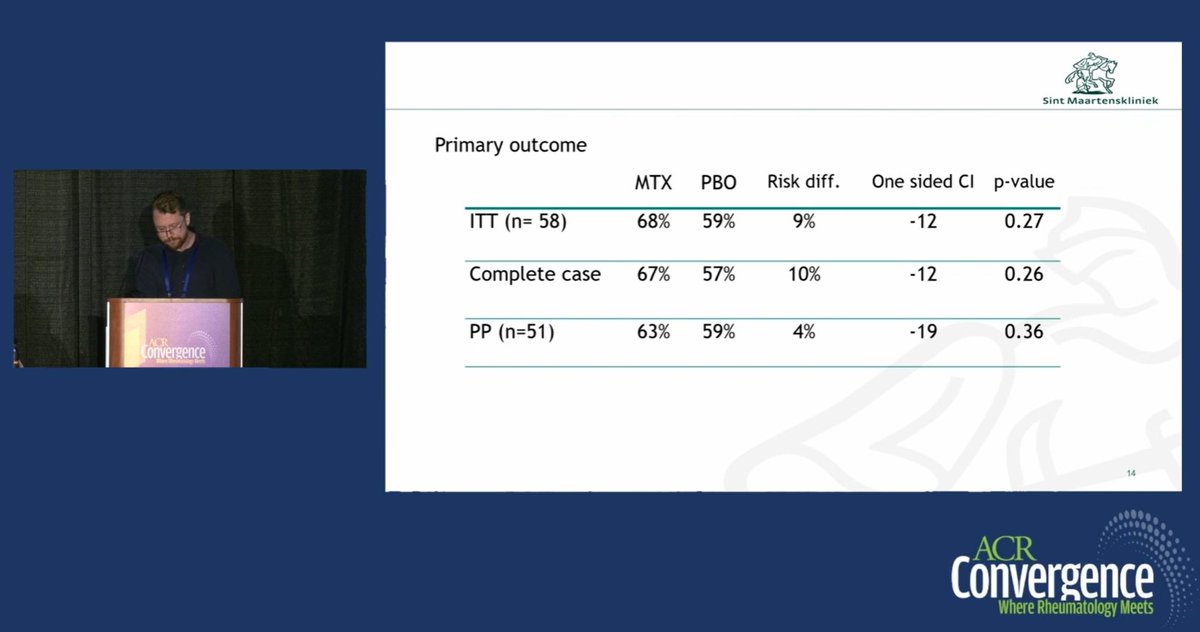
@drceowen @TheLancetRheum @RheumNow Efficacy in newly diagnosed & established PMR is not necessarily interchangeable
different treatment paradigm
?different immunologically
Many other diseases have different Rx for induction vs maintenance, early dx vs established.
Having said that: doesn't look great for MTX. https://t.co/89lByaYdYq


David Liew drdavidliew
1 year 2 months ago
Lot said about #ACR24 ABST1697:
MTX in newly diagnosed PMR, neg RCT
Many have said no hope for MTX in PMR now
Agree doesn't bode well
However, MTX may still have role in established PMR
@drceowen & I have made that call a priori @TheLancetRheum https://t.co/ywCJc0zHzC
@RheumNow https://t.co/JUXk2tDNyR

Janet Pope Janetbirdope
1 year 2 months ago
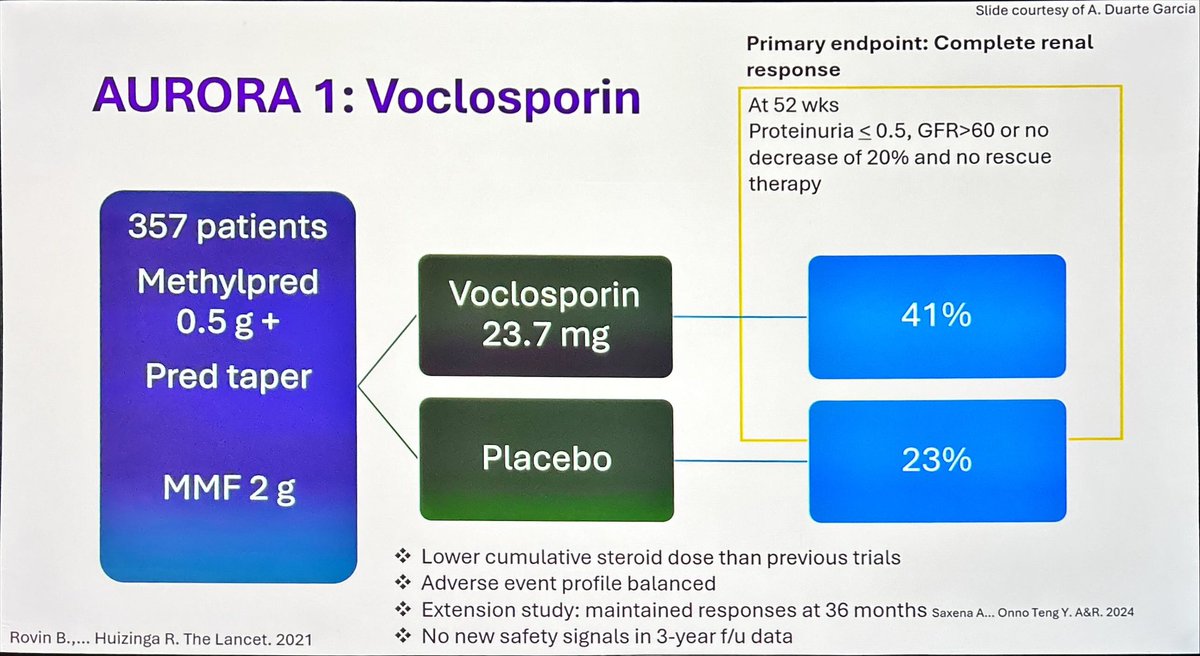
It is NO LONGER a ACCEPTABLE
To NOT consider
#MMF or #Cyclo + another proven #Rx
Added to
#HCQ and #tapering /limiting #glucocorticoids
RCTs in #lupus #nephritis support this
? Is which to add
#belimumab
#CNI #volclosporin
#obinutuzimab
#ACR #ACRbest @RheumNow @ACRheum https://t.co/a7WMFfCyXl

Dr. John Cush RheumNow
1 year 2 months ago
JAK-pot! How fast do DMARDs work?
Dr. Mike Putman interviews Dr. Kim Lauper about abstract 0501, How Fast Do JAK-inhibitors, TNF-inhibitors, Abatacept and IL-6 Inhibitors Act in Rheumatoid Arthritis? An International Collaboration of Registers of Rheumatoid Arthritis Patients… https://t.co/GO9EwyrVpV https://t.co/lELE5SJW5i

Highlights from Day 3 at ACR24 included the plenary session presentation on Nipocalimab (previously reviewed), but the big highlight was the Lupus Nephritis guideline recommendations.
This has been an interesting ACR meeting in terms of PMR updates. I would argue that we are still far too wedded to glucocorticoids only in the management of PMR. Yes, some patients will do fine with just glucocorticoids but we persist far too long with a glucocorticoid only strategy in others who clearly need an alternative as glucocorticoid adverse events multiply.

Dr. John Cush RheumNow
1 year 2 months ago
Continuing or Stopping Low Dose Glucocorticoids in GPA
Dr. Mike Putman reports about plenary session abstract 0774 (the TAPIR study) about how and when patients can stop steroids in GPA. #ACR24
https://t.co/OWqN0jmkc1 https://t.co/foOaVRtGiV


Richard Conway RichardPAConway
1 year 2 months ago
I've shared some thoughts on @RheumNow on methotrexate, tocilizumab, and baricitinib in PMR based on #ACR24 https://t.co/WXiW1nLN4k

Dr. John Cush RheumNow
1 year 2 months ago
Potential Impact of Weight Loss Drugs in Rheumatic Diseases
Dr. Arthur Kavanaugh highlights a session regarding weight loss and improvement in disease outcomes, specific weight loss drugs (SGL-2 and GLP-1), along with downsides when patients stop these medications. Reporting… https://t.co/Ilu2FXK2xi https://t.co/7CKSnfuey4

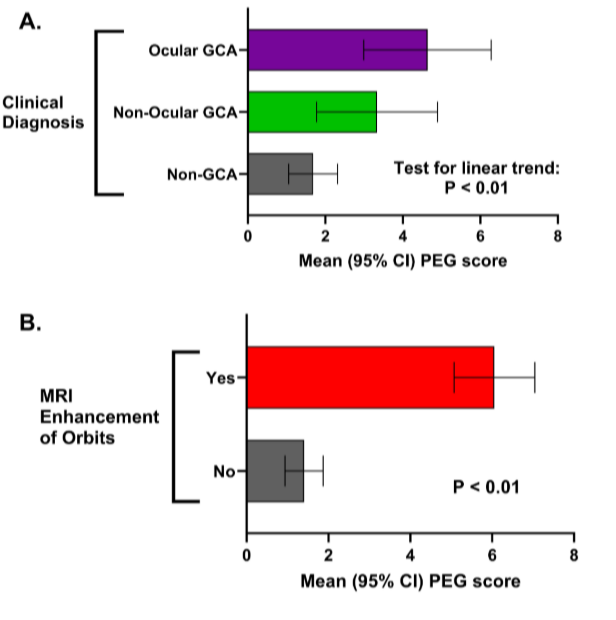
Richard Conway RichardPAConway
1 year 2 months ago
Yang et al. Cranial vessel wall MRI in GCA. Quantitated with PEG score. PEG score ocular GCA>non-ocular GCA>non-GCA. Decreases with treatment. @RheumNow #ACR24 Abstr#2650 https://t.co/e26urOpb7V https://t.co/eekQbzmKYm

Eric Dein ericdeinmd
1 year 2 months ago
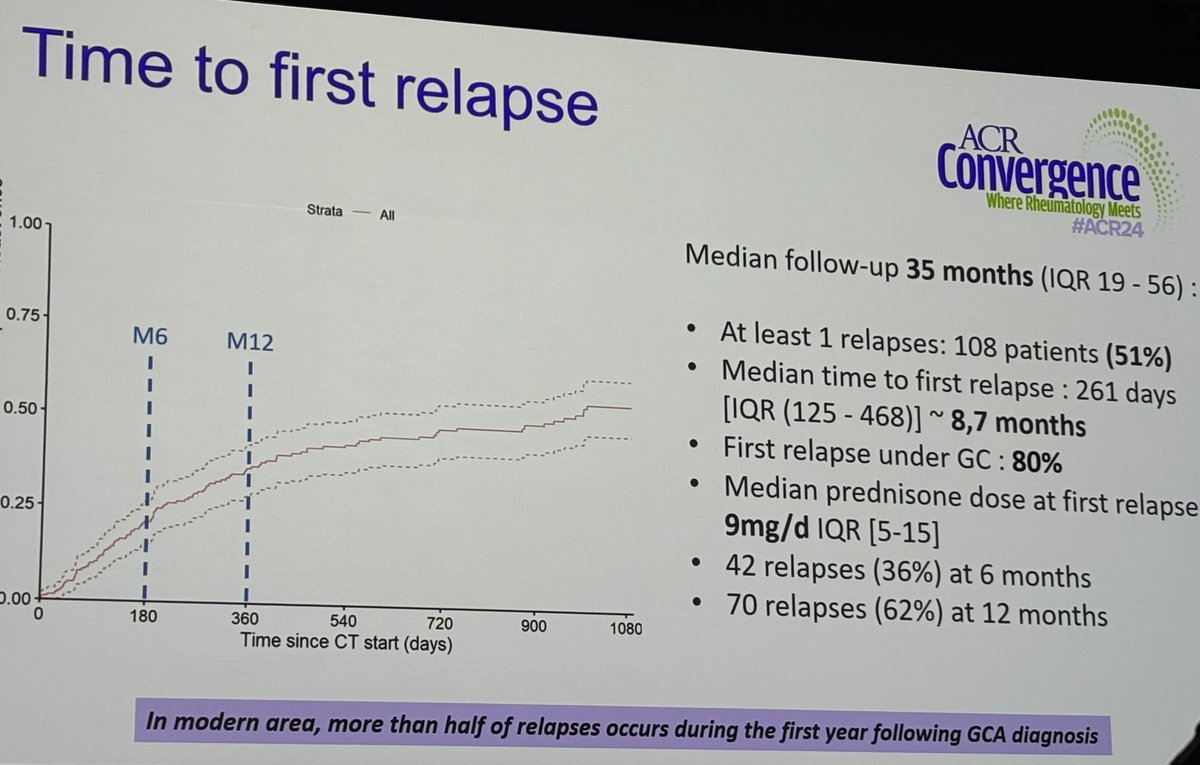
A#2652
NEWTON study 🇫🇷 Retrosp cohort
51% relapse. Median @8.7 mos, dose 9mg pred
Rf: limb art involv- HR 1.9
Pred taper speed not risk for relapse
Most relapse -> incr GCs
Toci 1/3 at dx, 50% stopped
-61% d/c due to remission, 39% SEs
-1/3 relapse after d/c
@RheumNow #ACR24 https://t.co/NP0wieDmvo

Richard Conway RichardPAConway
1 year 2 months ago
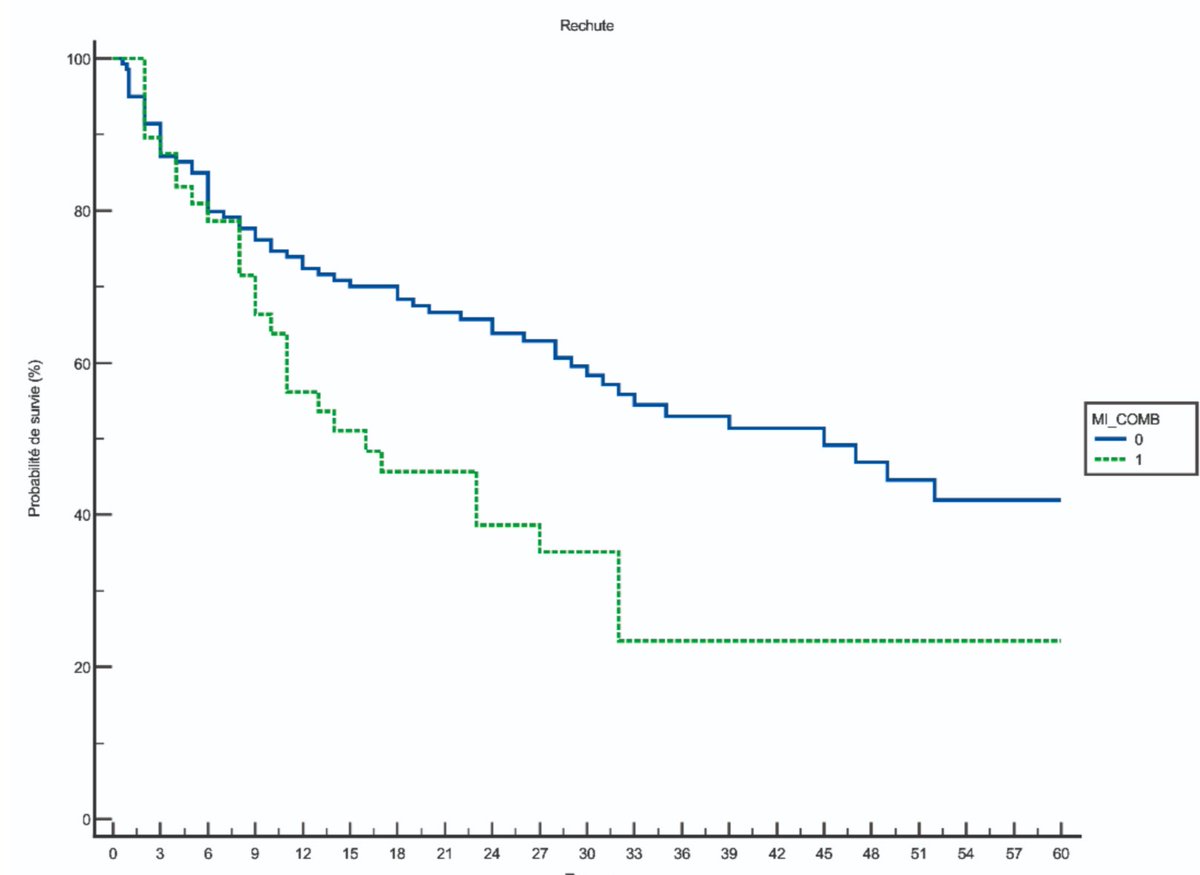
Peyrac et al. 211 GCA. Relapse in 52% at median 261 days (so 1st year). 83% on GCs at relapse, median dose 6.5mg pred. 36% relapse post-toc discontinuation, at median 133 days. 64% no relapse when toc stopped, at median 511 days @RheumNow #ACR24 Abstr#2652 https://t.co/NqtdDNGGoc https://t.co/mXD8x7O6Ww

Antoni Chan MD (Prof) synovialjoints
1 year 2 months ago
Study by Maria Dall'Era et al. compared voclosporin-based triple immunosuppressive therapy with high-dose GC in active lupus nephritis.
- Fewer adverse events in the voclosporin group, despite a higher incidence of specific issues like decreased GFR and hypertension.
- 25%… https://t.co/ToRu2rdErC https://t.co/uUXzNNuLDb














 Poster Hall
Poster Hall