Daily Recap - WEDNESDAY
Join panelists Drs. Janet Pope, Richard Conway, Meral El Ramahi and Jack Cush recap the best presentations presented on day four of the 2023 ACR Convergence meeting in San Diego, CA.
Watch video →Nov 10-15, 2023
Join panelists Drs. Janet Pope, Richard Conway, Meral El Ramahi and Jack Cush recap the best presentations presented on day four of the 2023 ACR Convergence meeting in San Diego, CA.
Watch video →Dr. Jonathan Kay discusses abstract 2148 with Dr. Josef Smolen at the 2023 ACR Convergence meeting in San Diego, CA.
Watch video →Dr. Atul Deodhar reporting on abstract 0519 from the 2023 ACR Convergence meeting in San Diego, CA.
Watch video →Dr. Arthur Kavanaugh discusses abstract 0025 at the 2023 ACR Convergence meeting in San Diego, CA.
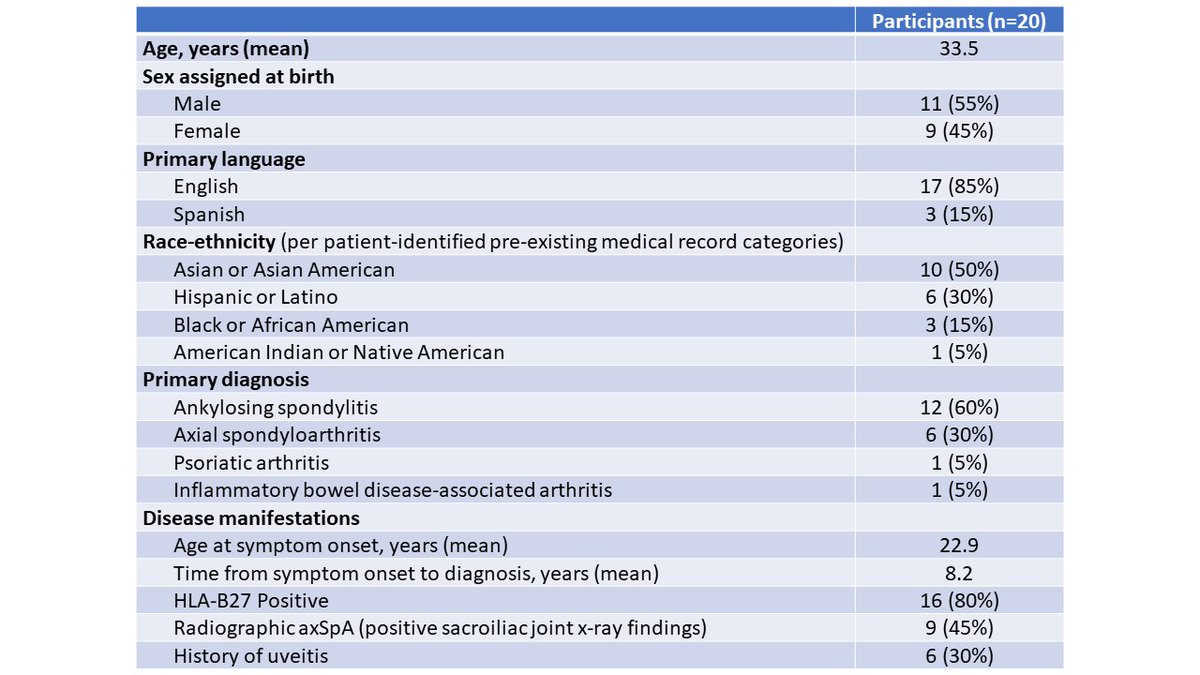
Watch video →Dr. Rachel Tate and Dr. Catherine Blakewell discuss treatment options patients in spondyloarthritis at the 2023 ACR Convergence meeting in San Diego, CA. Abstracts discussed include 0520, 0530, 0521 and 0529.
Watch video →Dr. Jack Cush discusses abstract 2427 presented at the 2023 ACR Convergence meeting in San Diego, CA.
Watch video →Dr. Jack Cush and Dr. Janet Pope at the 2023 ACR Convergence meeting in San Diego, CA.
Watch video →Dr. Peter Nash reports on abstracts 0514 and 0538 from the 2023 ACR Convergence meeting in San Diego, CA.
Watch video →Dr. Peter Nash discusses a study that looks at the window of opportunity for treatment of PsA at the 2023 ACR Convergence meeting in San Diego, CA.
Watch video →Dr. Jack Cush and Dr. Janet Pope discuss abstract 1584 presented at the 2023 ACR Convergence meeting in San Diego, CA.
Watch video →Dr. Peter Nash reports on abstract 1691 presented at the 2023 ACR Convergence meeting in San Diego, CA.
Watch video →Dr. Jack Cush discusses abstract 1583 presented at the 2023 ACR Convergence meeting in San Diego.
Watch video →Dr. Mike Putman discusses abstract 0725 with Dr. Sophie Nagle at the 2023 ACR Convergence meeting in San Diego, CA.
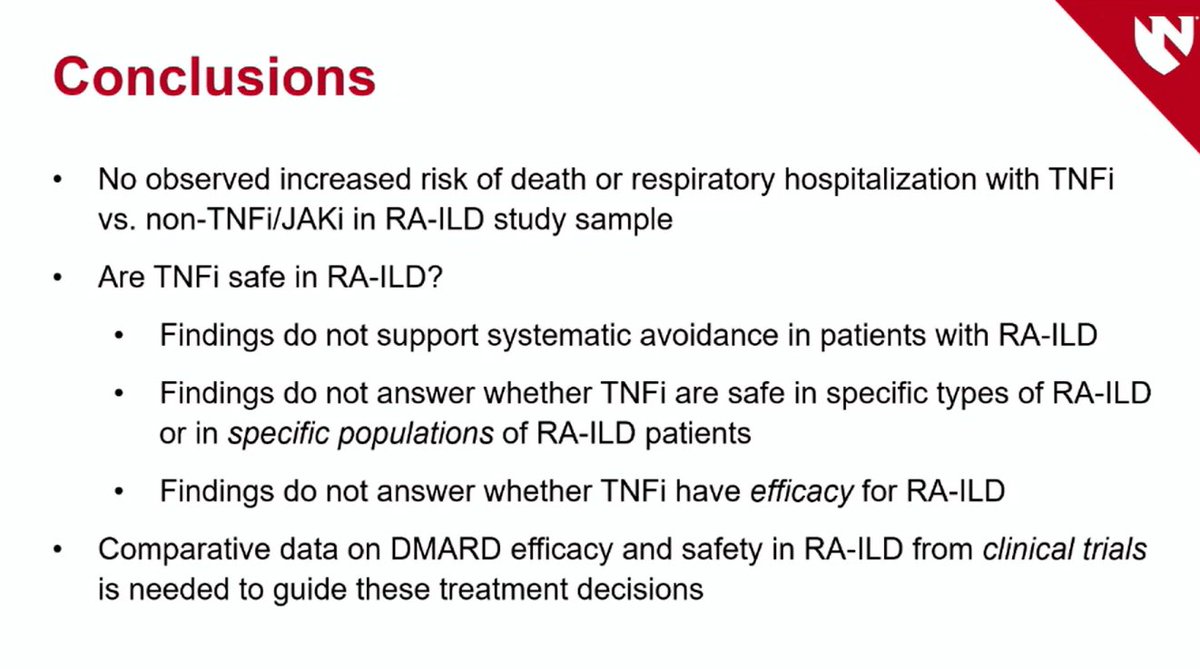
Watch video →Cancer risk minimisation is a high priority for people with rheumatic diseases, as it is for the general population. Tumor necrosis factor inhibitors (TNFi) have a long history of association with cancer risk discussions. An oral presentation by Suarez-Almazor et al provided more supportive data on using TNFi in this population.
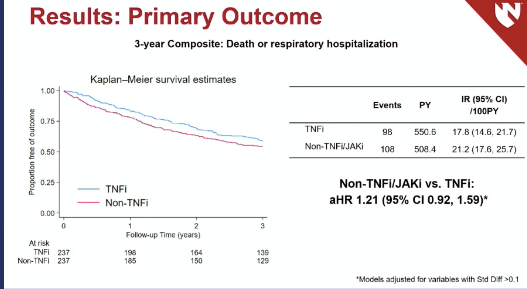
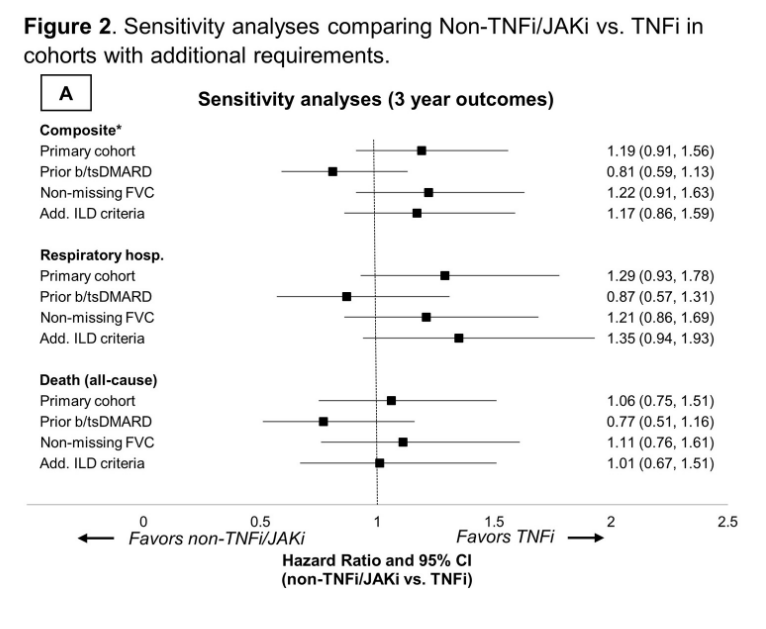
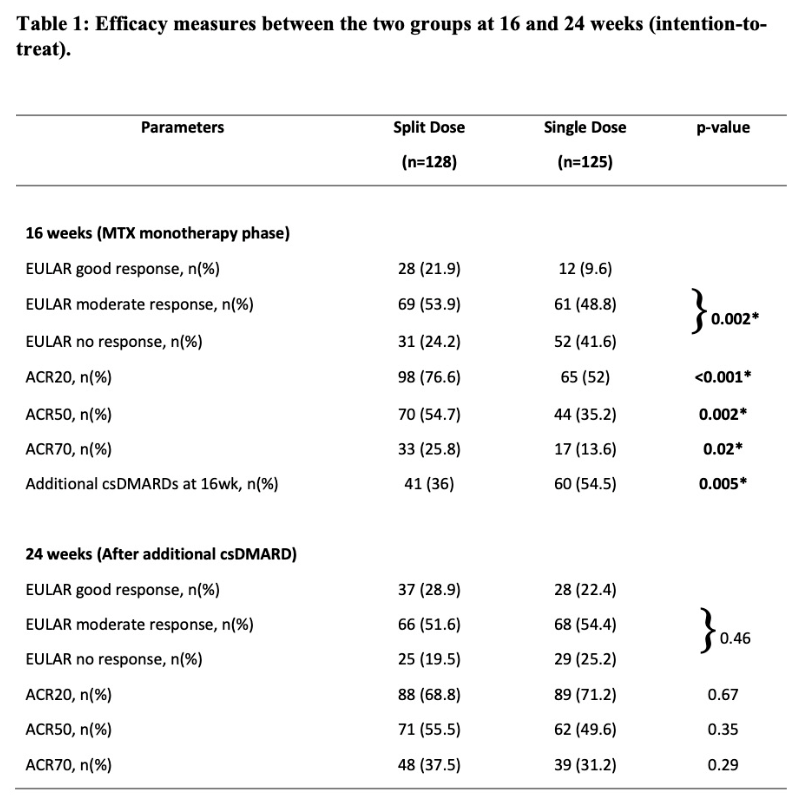
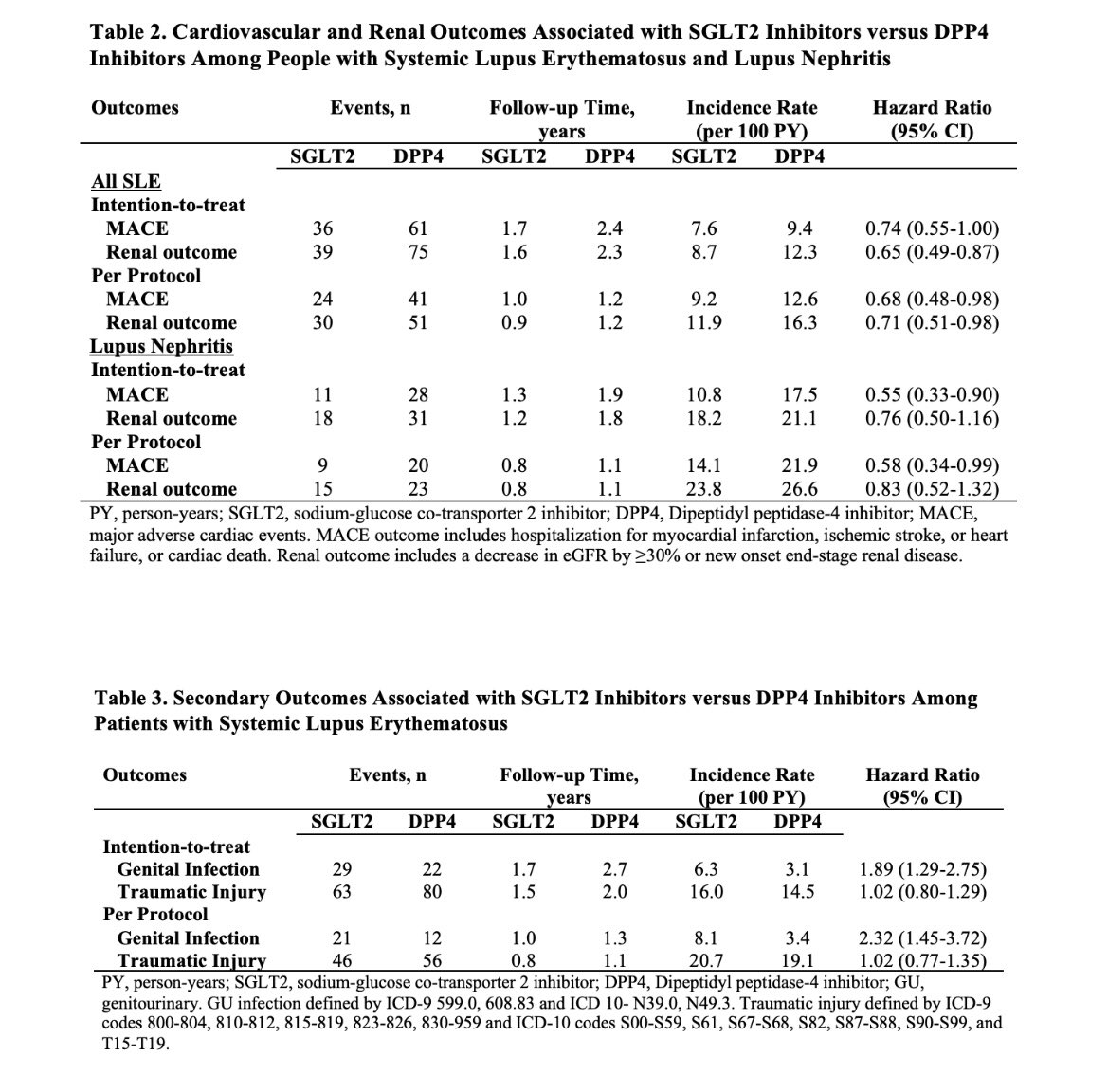
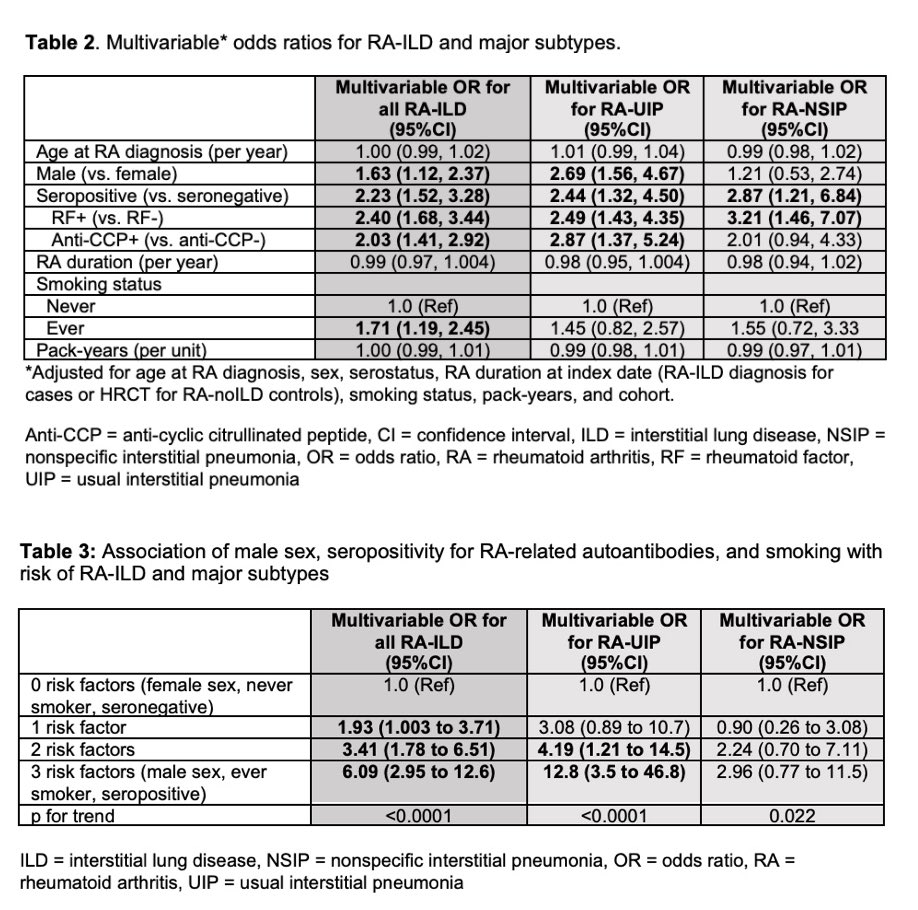
Read more →Our reporters have been prolific in finding the hot abstracts, those that were most attended or those that are getting the most buzz on social media. Here are RheumNow's #ACRbest abstract reports from Monday, November 13, 2023 at #ACR23, covering The Great Debate, SGLPT2 inhibitors in SLE, the SMART Study of MTX, TMP/SMX Prophylaxis, RA-ILD & TNF Inhibitors, cancer research and more.
Read more →Dr. Peter Nash discusses abstract 1414 at the 2023 ACR Convergence meeting in San Diego, CA.
Watch video →Drs. Jack Cush and Kevin Winthrop discuss COVID 19 at 2023 ACR Convergence in San Diego, CA.
Watch video →Dr. Eric Dein talks with Dr. Philip Seo, one of two panelists for the Great Debate: Should PMR and GCA Be Treated with Advanced Therapies at Disease Onset? at the 2023 ACR Convergence meeting in San Diego, CA.
Watch video →














By downloading this material, I acknowledge that it may be used only for personal use and personal education and that I will accredit RheumNow.com as the source and owner of this material. Commercial use or mass reproduction of this material without permission from RheumNow (info@rheumnow.com) is prohibited.