Autoinflammatory
In comments submitted to the Centers for Medicare and Medicaid Services (CMS) in response to the CY 2023 Medicare Physician Fee Schedule and Quality Payment Program proposed rule, the American College of Rheumatology applauded proposals that would provide more flexibility and improve care coordination, while raising concerns about proposed cuts to reimbursement for critical services provided by rheumatologists and other cognitive specialists.
Dr. Jack Cush discusses declining survival rates in the USA, FDA approvals of new COVID subvariant boosters and other odd and possibly true new research reports from the past week on RheumNow.com.
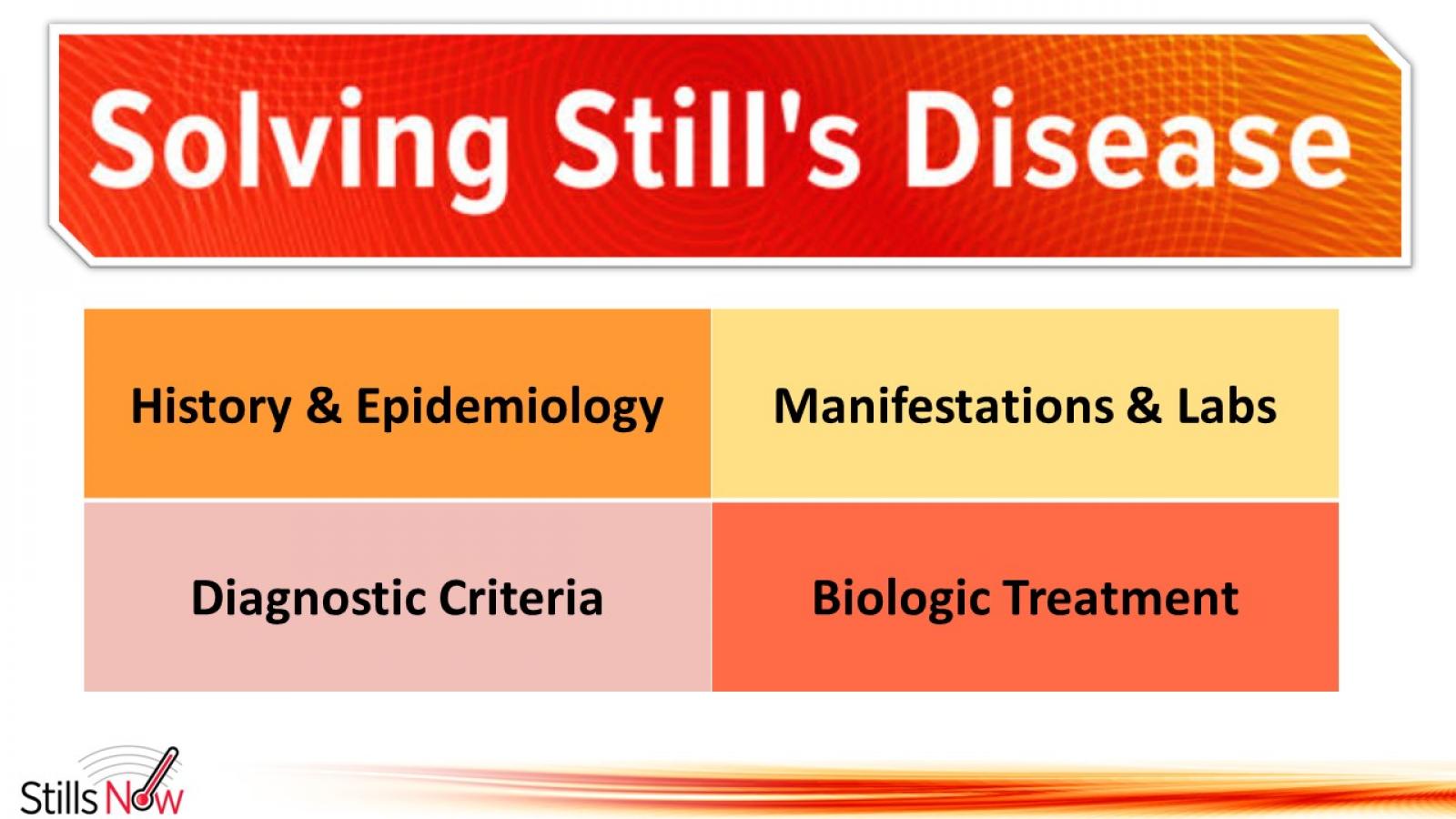
Not all patients with periodic fevers fit neatly into diagnostic categories. Some can be diagnosed as Still’s disease (based on criteria) while others can be classified as autoinflammatory diseases (AID) and some may be unclassifiable, clinically or genetically.
Still's disease in adults (AOSD) or children (sJIA) can have dramatic symptom severity, making it easy to gauge disease activity and response to therapy, especially at the outset. However, a validated measure of disease activity has not been agreed (for clinical trial and treatment assessments). A new study compares two such activity measuresin a large cohort of Still's patients.
A cohort analysis from Toronto suggests that axial psoriatic arthritis (PsA) is distinctly different from axial ankylosing spondylitis (AS) with psoriasis.
Researchers examined two PsA and AS cohorts - patients with PsA with axial disease and isolated axial patients with AS with psoriasis.
A small retrospective study suggests that patients with difficult to treat adult-onset Still's disease (AOSD) or sytemic juvenile idiopathic arthritis (sJIA) may respond well to JAK inhibitor (JAKi) agents - presumable by blocking pro-inflammatory cytokines, notably IL-6 and IFN.
Your patient doesn't meet criteria for Still’s disease (AOSD or sJIA), now what should you do or consider?
What you do or consider next can be addressed according to the stage of current disease: A) Hospitalized Febrile Disease, or B) Outpatient “Still’s” Disease.
Fever of unknown origin (FUO) represents a diagnostic challenge to many physicians and while cancer and infectious causes need to be excluded, rheumatic disorders are amongst the most common causes of FUO.
A recent metanalysisi of the medical literature from 2002 to 2021, included studies with ≥50 patients reporting on causes of FUO/IUO (inflammation of unknown origin). This series included 16884 patients.
There is no “test” (blood or other) that is solely diagnostic of Still’s disease, but labs can help make a diagnosis or manage disease, and affirm the safety of drugs in use.
Still’s disease is a rare inflammatory disorder, affecting less than 1 person per 2000 people. This disease may occur in both children and adults, namely as systemic juvenile idiopathic arthritis (sJIA) and adult-onset Still’s disease (AOSD).
The paediatric form was described by George Still in 1896, whereas the adult variant later by Eric Bywaters in 1971. However only the adult disease is identified by the name of Still.
Are you treating “systemic” or “articular” (arthritis) Still’s disease? Most Still’s patients have a dominance of one or the other. With certainty, the right therapy for the right symptoms can be chosen. What about patients who have an incomplete or no response, or who become unresponsive to a drug that once worked well?
Dr. Jack Cush covers the news and journal reports from the past week on RheumNow.com. This week we have Insights NAFLD, overdose deaths, septic arthritis, refractory stills, & when MTX doesn’t work.
The concept of a “Still’s disease continuum” that encompasses both sJIA and AOSD is based on the many common clinical, genetic and laboratory features shared by both sJIA and AOSD.
Many clinicians may not have seen a case of AOSD during training, which overall leads to several delays in referrals and appropriate diagnosis for AOSD patients. AOSD is an autoinflammatory disease where innate immunity plays a primary role and is characterized by seemingly unprovoked inflammation, but without the high-titer autoantibodies or antigen specific T cells seen in autoimmune diseases.
Dr. Jack Cush reviews the new studies and drug approvals and new insights into febrile disorders from the past week on RheumNow.com
Ustekinumab (IL-12/23i) phase 2 study was successful in #SLE; but the phase 3 LOTUS study of 512 pts, UST was NOT superior to PBO (SRI-4 44% v 56%) at 1 year. Study was halted for lack of efficacy (but no safety concerns). https://bit.ly/3RvPzDm




















 Poster Hall
Poster Hall