Drug Safety
Your patient doesn't meet criteria for Still’s disease (AOSD or sJIA), now what should you do or consider?
What you do or consider next can be addressed according to the stage of current disease: A) Hospitalized Febrile Disease, or B) Outpatient “Still’s” Disease.
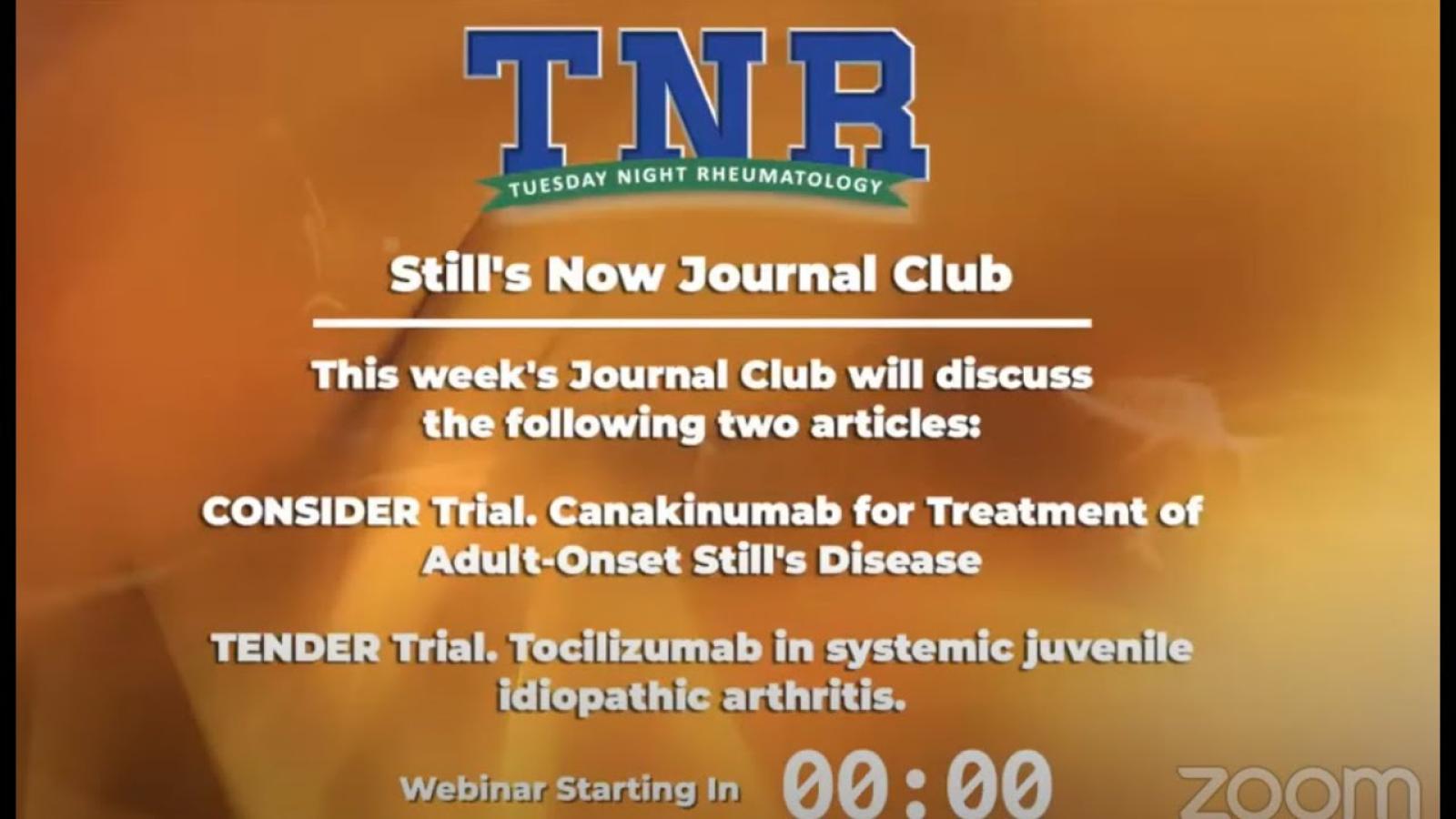
Dr. Jack Cush reviews the news, journal reports and rheumatologist cases from the past week on RheumNow.com. This podcast is brought to you by StillsNow.com - be sure to sign up for our monthly StillsNow email and Monthly StillsNow Podcast.
Mehta et al have published a full read review of managing interstitial lung disease (ILD) in patients with inflammatory myopathies, a heterogeneous group of syndromes connected by ILD and and increased morbidity and mortality risk.
They divide myositis-ILD into three main prognostic groups with different treatment approaches:
There is no “test” (blood or other) that is solely diagnostic of Still’s disease, but labs can help make a diagnosis or manage disease, and affirm the safety of drugs in use.

Dr. John Cush RheumNow
3 years 5 months ago
Have you checked out our new sister-site, Still's Now? A new site for Still's disease, autoinflammatory & febrile disorders.
https://t.co/oWEugnOB6k https://t.co/5jwiP2Xqrz

Management of arthralgias before a certified rheumatoid arthritis (RA) diagnosis is challenging - should one use DMARD therapy before clinically evident synovitis in a preemptive effort to avoid or forestall the diagnosis or damage of RA?

Dr. John Cush RheumNow
3 years 5 months ago
11.5% of Crohns pts have TNFi use contraindications (either MS, CHF, neoplasia, infx risk, TNFi AE, comorbidities, SLE. Alternatively GI survey respondents use ustekinumab (76%), vedolizumab (249%), or tofacitinib (0.5%) https://t.co/6ApUz93iS0 https://t.co/PTmnsTd2Wh

Dr. John Cush RheumNow
3 years 5 months ago
Overdose deaths increased to 107 000 deaths in US in 2021, with significant racial disparity. Higher overdose rates seen in American Indian, Alaska Natives and Blacks. WORSE during COVID - 2020, overdose rates were 7 times higher in Blacks than Whites https://t.co/PMRo9gbzZl https://t.co/CgxgemyEA7
Are you treating “systemic” or “articular” (arthritis) Still’s disease? Most Still’s patients have a dominance of one or the other. With certainty, the right therapy for the right symptoms can be chosen. What about patients who have an incomplete or no response, or who become unresponsive to a drug that once worked well?

Dr. John Cush RheumNow
3 years 5 months ago
Rheums: Got a Rheumatology question or case for Jack Cush? Record it here and we'll feature it on an upcoming podcast. Tell us your name and where you practice rheumatology.
https://t.co/QUTIbK3r89 https://t.co/FZcTLREida
Dr. Jack Cush covers the news and journal reports from the past week on RheumNow.com. This week we have Insights NAFLD, overdose deaths, septic arthritis, refractory stills, & when MTX doesn’t work.

Dr. John Cush RheumNow
3 years 5 months ago
Rheumatologist Survey:
What do you rely on MOST in diagnosing Still’s disease?
Sxs? Labs? Both? Criteria? Fever?
Vote here:
https://t.co/oANKpKqJA5 https://t.co/LIjRSBHNBi

Dr. John Cush RheumNow
3 years 5 months ago
2015 NEJM study of 4g acetaminophen vs PBO in 700 critically ill ICU patients with fever ≥38°C, showed Tylenol vs PBO had no differences in mortality, ICU stay or LFTs. Tylenol had small but signif reduction in Temp (38.4±1.0°C vs. 38.6±0.8°C; P<0.001) https://t.co/qnHgFRp20M https://t.co/2E4ZEsIFUV

A large prospective psoriatic arthritis (PsA) study examined the enthesitis outcomes when PsA patients received conventional (cDMARDs) or targeted disease-modifying antirheumatic drugs (tDMARDs) and showed an overall 86% response rates, regardless of the medication used.















 Poster Hall
Poster Hall