Rheumatoid Arthritis
The window of opportunity concept in RA shifted our focus to trying to treat disease earlier and more aggressively to improve long term outcomes. A natural development of this was to reconsider the possibility of therapeutic interventions aimed at the prevention of rheumatoid arthritis.
In clinical practice, pulmonary manifestations of rheumatic medical diseases such as rheumatoid arthritis (RA), psoriatic arthritis (PsA), and peripheral spondyloarthritis (pSpA) are typically not screened for upon diagnosis of a rheumatic disease in patients without any signs or symptoms suggestive of pulmonary involvement.
Since the millennium, we have seen an expansion in the number of advanced treatments both biologic and targeted synthetic disease modifying anti-rheumatic drugs for rheumatoid arthritis. The challenge remains on how best to characterise the subtypes of RA in order to choose the best drug to ensure optimal outcome for patients.
Research work from the Accelerating Medicines Partnership (AMP: RA/SLE) Network, was published in Nature and more specifically characterizes RA synovium into several cell-type abundance phenotypes (CTAPs). Could CTAPs known disease features or more effective future therapies?
A recent CDC reports estimates that in 2019–2021, 21% of U.S. adults (53.2 million) have physician diagnosed arthritis. Now, an updated report shows a larger number (~33%) of U.S. veterans having diagnosed arthritis. Compared to nonveterans, this prevalence was double in men, and 60% higher in women.
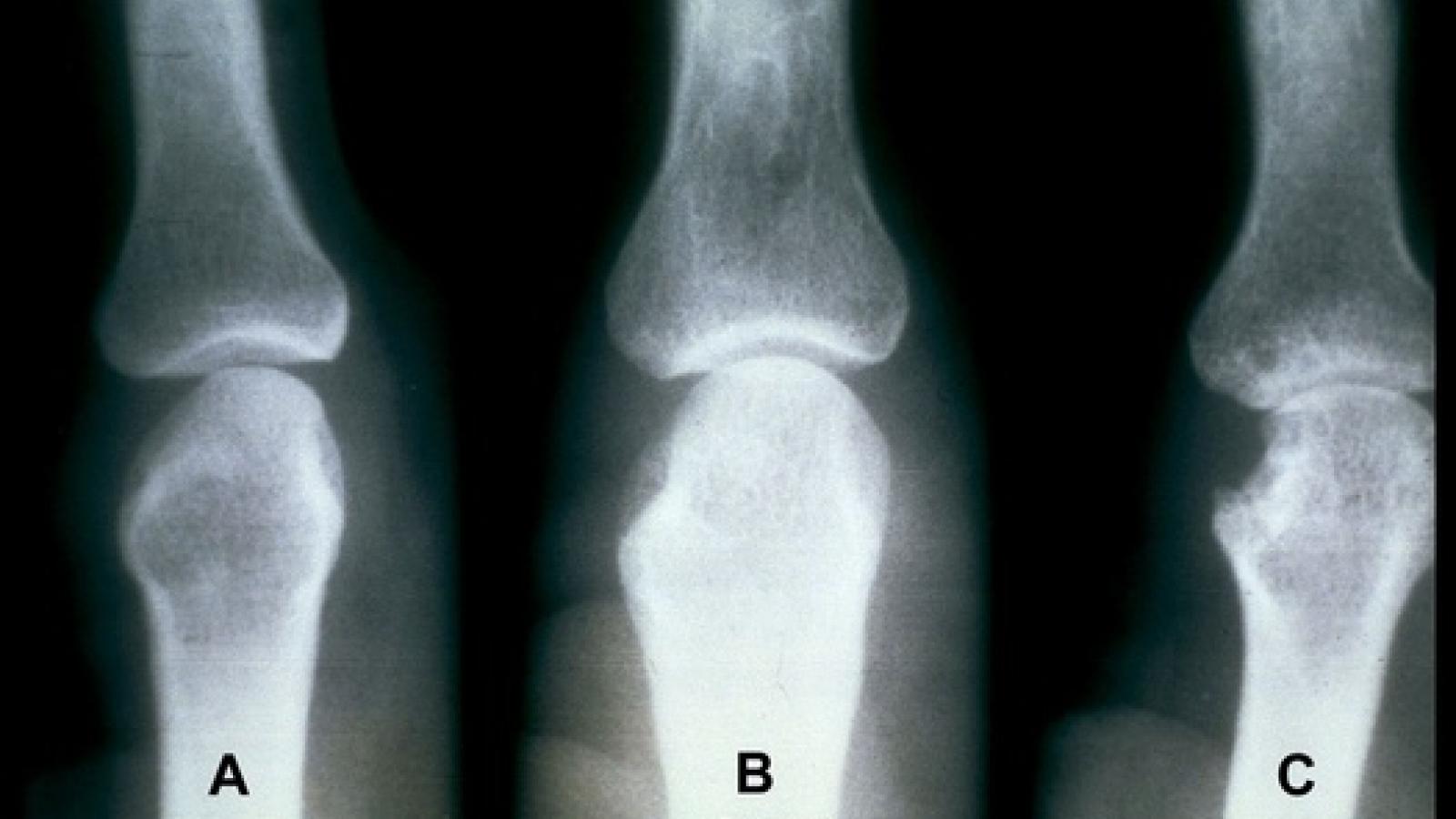
The American College of Rheumatology's (ACR) has published a preview of new research from ACR Convergence 2023 showing that AI and a deep learning system could accurately identify and predict joint space narrowing and erosions in hand radiographs of patients with rheumatoid arthritis (RA).
Routine hand and foot radiographs in more than 700 patients being evaluated for rheumatoid arthritis (RA) made almost no difference in diagnosing the condition nor in predicting its course, Dutch researchers said.
A study of nearly 80,000 US veterans who underwent primary knee joint arthroplasty (TKA) showed the incidence of prosthetic joint infection (PJI) was highest in the first 3 months and remained elevated through 12 months compared with 12 months or more after surgery. Gram-negative organisms were more prevalent in early vs delayed or late PJIs.
A prospective study of first line use anakinra in systemic juvenile idiopathic arthritis (sJIA) proved to be effective and without potentially allergic lung reactions.
Dr. Jack Cush reviews the news, journal reports and regulatory approvals from the past week on RheumNow.com.
Study of LATE-onset RA (>65y), shows DMARD initiation is low in LORA; despite current clinical practice guidelines recommending early aggressive Rx. Among 3,373 LORA pts (age77 yrs), only 29% initiated on a DMARD. https://bit.ly/47dT6x6



















 Poster Hall
Poster Hall