Dr. Jack Cush covers the news and journal reports from the past week on RheumNow.com. This week we have Insights NAFLD, overdose deaths, septic arthritis, refractory stills, & when MTX doesn’t work.
Patients and their family for years have been inviting me to their dinners, picnics, baptisms, anniversaries, and funerals. I always felt somewhat awkward when asked to participate in a patient’s life outside of my office or the hospital setting and usually will decline politely. I tell myself I should not blur the lines between patient care and friendship.
I broke this rule recently.
A large prospective psoriatic arthritis (PsA) study examined the enthesitis outcomes when PsA patients received conventional (cDMARDs) or targeted disease-modifying antirheumatic drugs (tDMARDs) and showed an overall 86% response rates, regardless of the medication used.
The concept of a “Still’s disease continuum” that encompasses both sJIA and AOSD is based on the many common clinical, genetic and laboratory features shared by both sJIA and AOSD.
Placebo responses are to be expected in rheumatoid arthritis (RA) clinical trials, but are such placebo responses affected by continuing background DMARDs like methotrexate (MTX) even though there was an inadequate response (IR) to MTX?
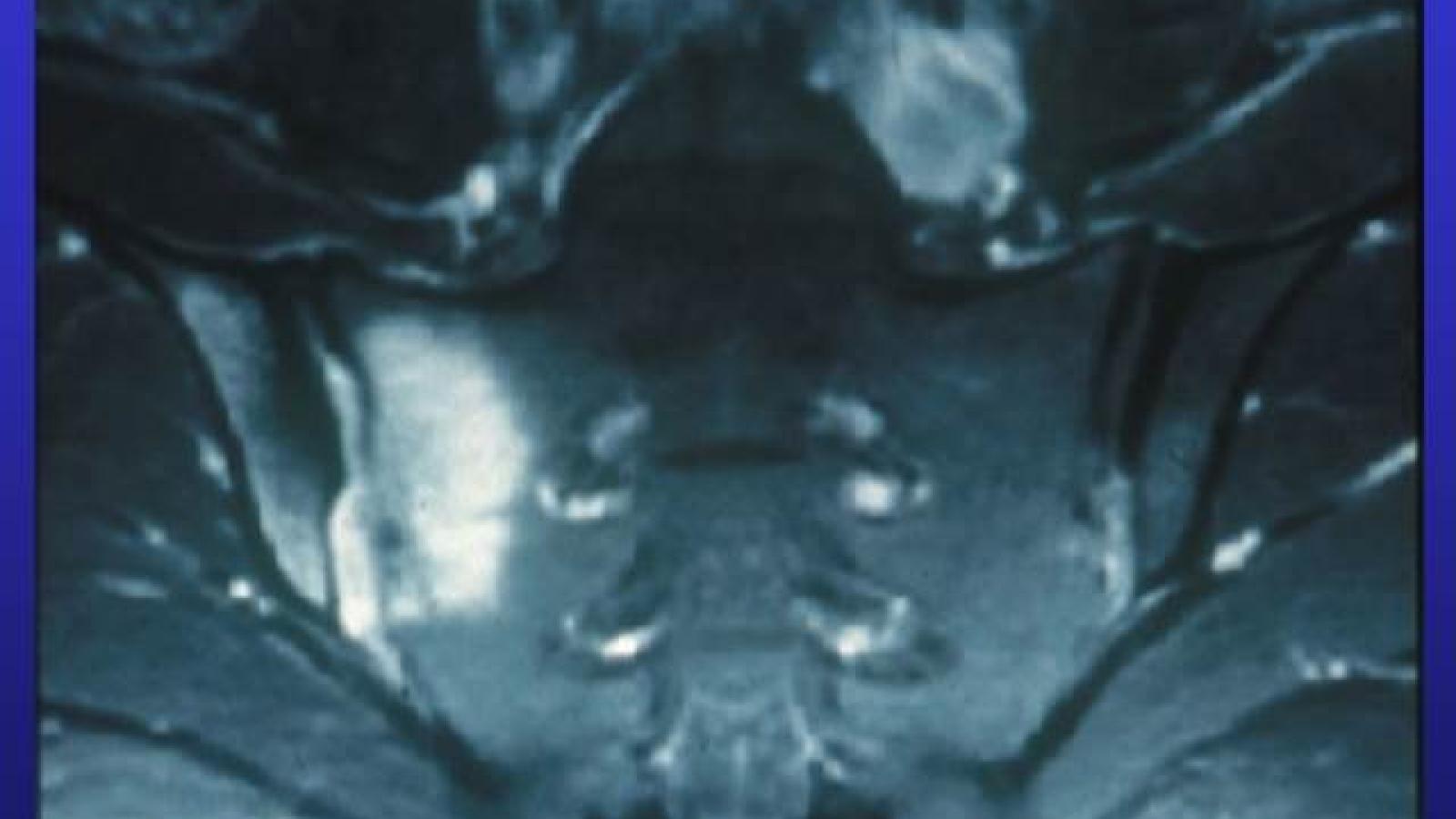
For about one in six people considered healthy with no reports of back pain, lesions were visible on MRI in the lower spinal column and sacroiliac joint, researchers said -- a sign that rheumatologists should be cautious about diagnosing spondyloarthritis (SpA) on the basis of imaging.
An open-label, 2 year study evaluated the efficacy and safey (drug retention) of subcutaneous (SC) abatacept (ABA) in active rheumatoid arthritis (RA) and showed superior responses when ABA was given to biologic-naive and seropositive RA patients.
Many clinicians may not have seen a case of AOSD during training, which overall leads to several delays in referrals and appropriate diagnosis for AOSD patients. AOSD is an autoinflammatory disease where innate immunity plays a primary role and is characterized by seemingly unprovoked inflammation, but without the high-titer autoantibodies or antigen specific T cells seen in autoimmune diseases.
Dr. Jack Cush reviews the new studies and drug approvals and new insights into febrile disorders from the past week on RheumNow.com
Ustekinumab (IL-12/23i) phase 2 study was successful in #SLE; but the phase 3 LOTUS study of 512 pts, UST was NOT superior to PBO (SRI-4 44% v 56%) at 1 year. Study was halted for lack of efficacy (but no safety concerns). https://bit.ly/3RvPzDm
Antimalaria (AM) therapy is a cornerstone to the management of systemic lupus erythematosus (SLE), yet a recent study suggests that slowly tapering AM yields a lower rate of SLE flares.
What is the classic 'triad' of Still's disease? Does it affect males and females equally? What are typical lab findings? Which drugs are effective at treating Still's, and as importantly, which ones are not? What about complications? Read on for these and other FAQs regarding Still's disease.
A large cohort study of children with febrile disorders has demonstrated the diagnostic utility of Myeloid-related protein 8/14 (MRP8/14) in diagnosing systemic JIA patients (SJIA) in clinical practice.
A cohort study suggests that rituximab (RTX) use among patients 75 years and older with antineutrophil cytoplasmic antibody (ANCA)–associated vasculitis (AAV) is efficacious but also has a high risk of serious adverse events, likely related to associated steroid use and the advanced age of the population.
The BMJ has published the results of a metanalysis showing strong conclusive evidence that viscosupplementation in knee osteoarthritis (kOA) has minimal effects on kOA pain, and also reveals strong evidence of an increased risk of serious adverse events.
Adding a corticosteroid shot to exercise therapy significantly improved symptoms of chronic Achilles tendinopathy, a 100-person randomized trial found.
































 Poster Hall
Poster Hall