All News
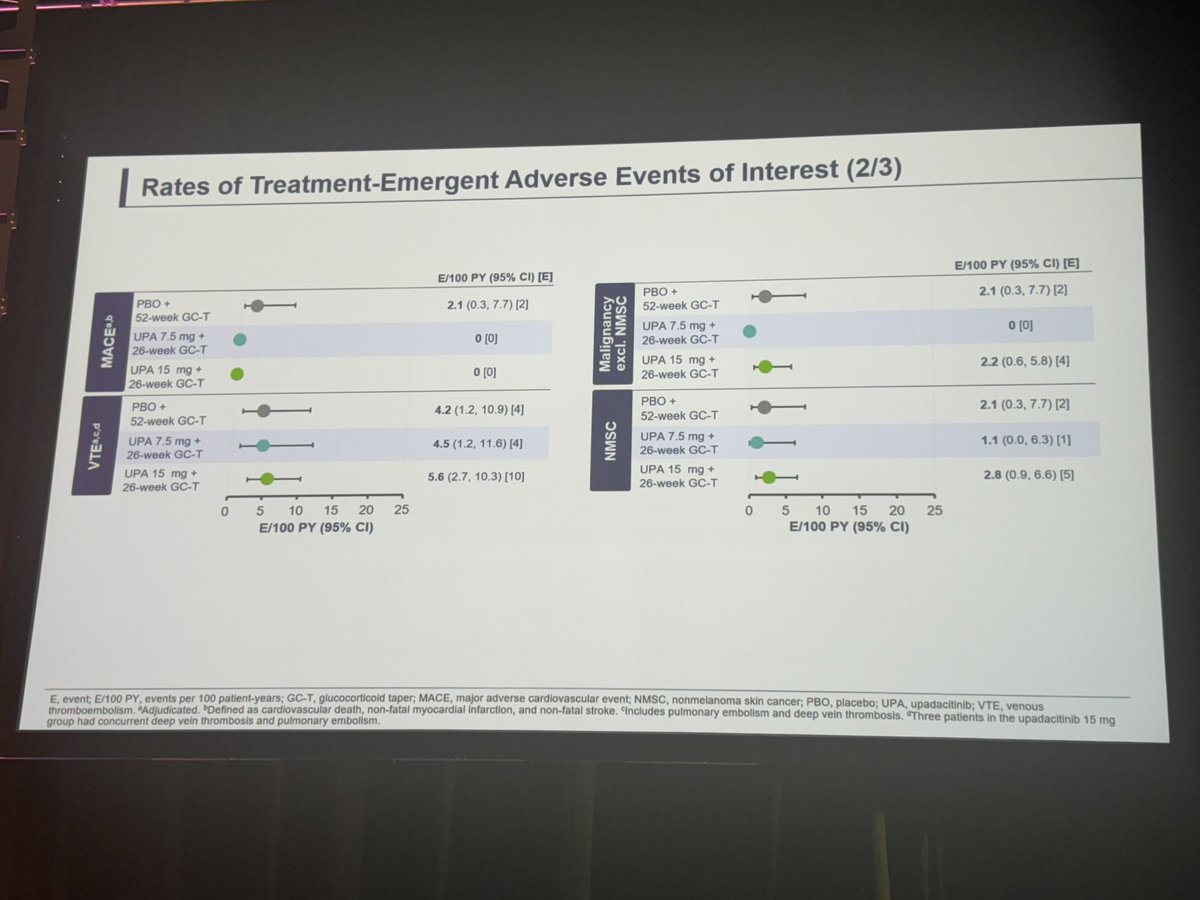
Safety data reassuring with UPA 15 mg vs PBO
No UPA MACE events, low VTE
Ab#0770
@RheumNow #ACR24 https://t.co/lMf2dCz2RX https://t.co/3DnPIoVOt8
Links:
Eric Dein ericdeinmd ( View Tweet)

Planned to post so much more from #ACR24; my favorite slides from today will have to suffice.
From the #BCRC Dr Monica Guma’s - diet and microbiome.
Dr @NamrataRheum -a reminder that we are all aging.
Dr Connie Weyand’s -metabolic checkpoints in RA T cells and macrophage. https://t.co/MtsheVsUEQ
Links:
Kristen Young kristenyoung ( View Tweet)

Hypophosphatasia:
🦴Inherited disorder of metabolism with low tissue nonspecific alkaline phosphatase (TNSALP)
🦴Impaired bone mineralisation
🦴Accumulation of pyrophosphate
🦴1/100,000-300,000
🦴6 main forms
@RheumNow #ACR24
Mrinalini Dey DrMiniDey ( View Tweet)
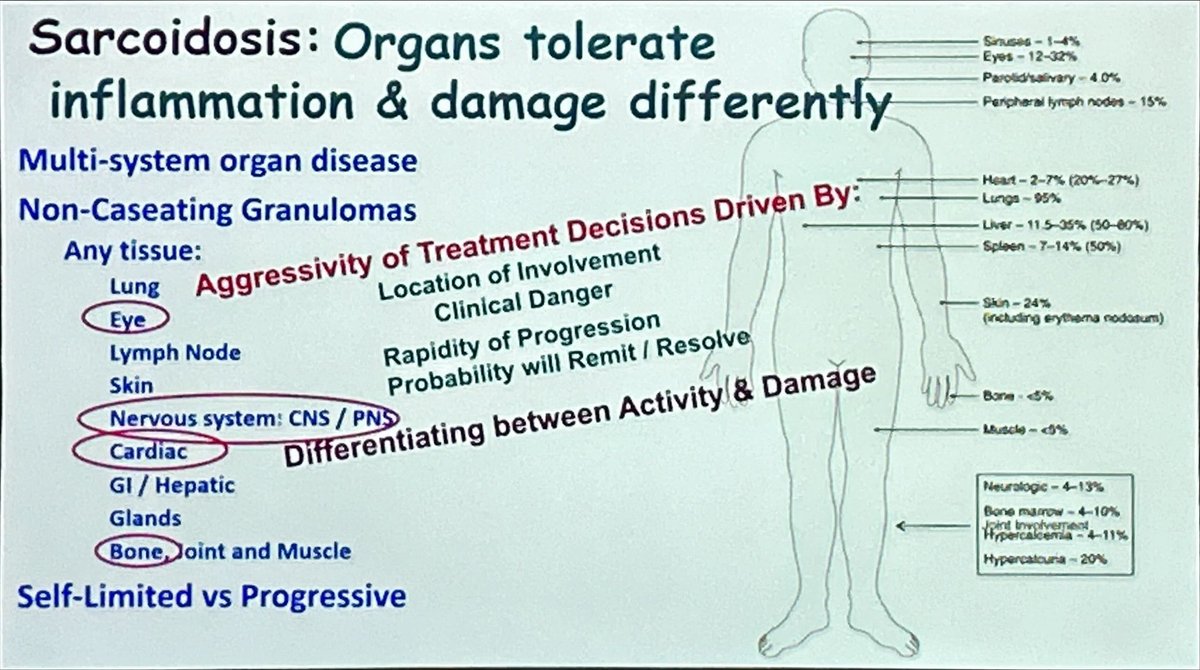
Différent patterns of organ involvement in sarcoidosis @RheumNow #ACR24 #Sarcoidosis https://t.co/xigkS3vpUh
Antoni Chan MD (Prof) synovialjoints ( View Tweet)
Sarcoid - diagnosis of probability!
Biopsy not required! Can be bx-supported, not confirmed!
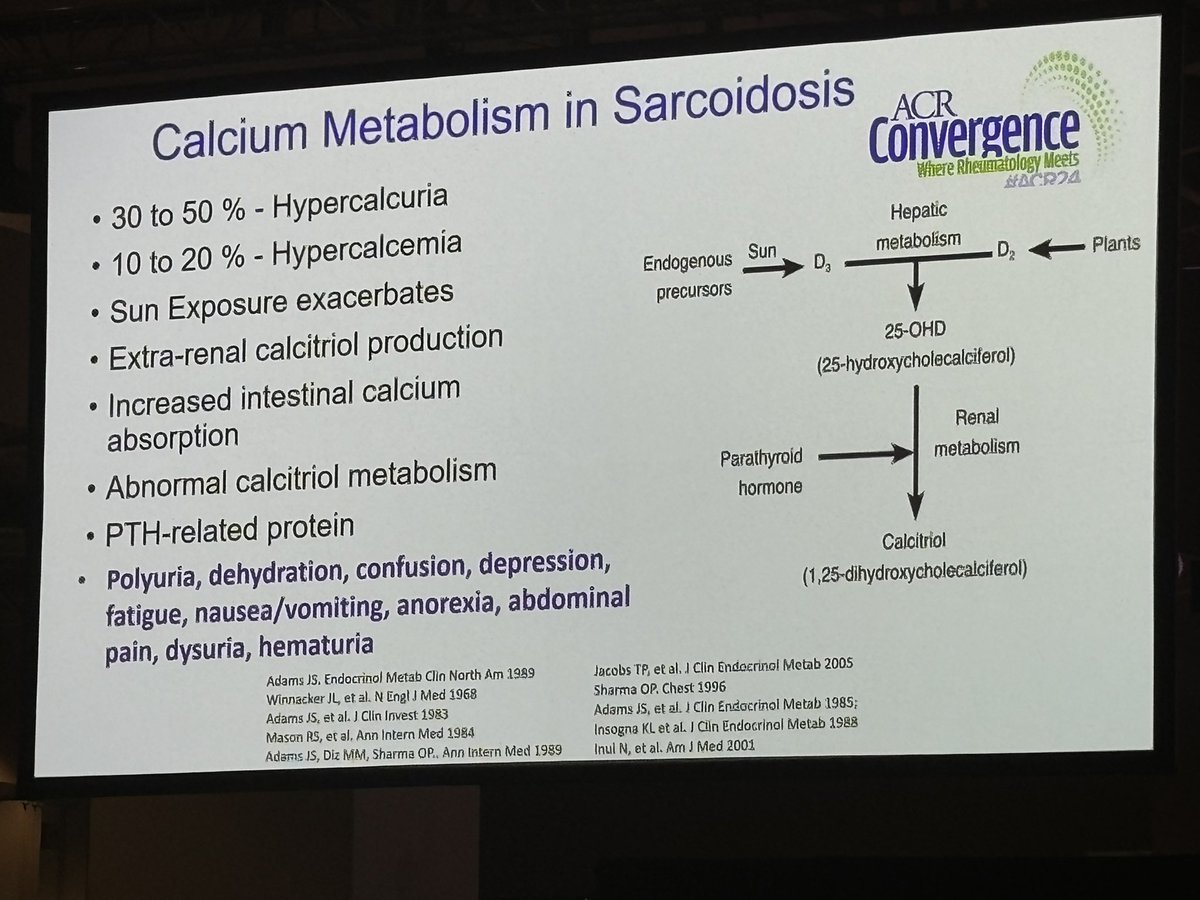
Calcium in Sarcoid
10-20% hypercalcemic
30-50% hypercalcuria
Sc: polyuria, dehydration, confusion, depression, fatigue, n/v, anorexia, abd pain, hematuria
@RheumNow
#ACR24 Rev Course https://t.co/B1srD3saij
Eric Dein ericdeinmd ( View Tweet)
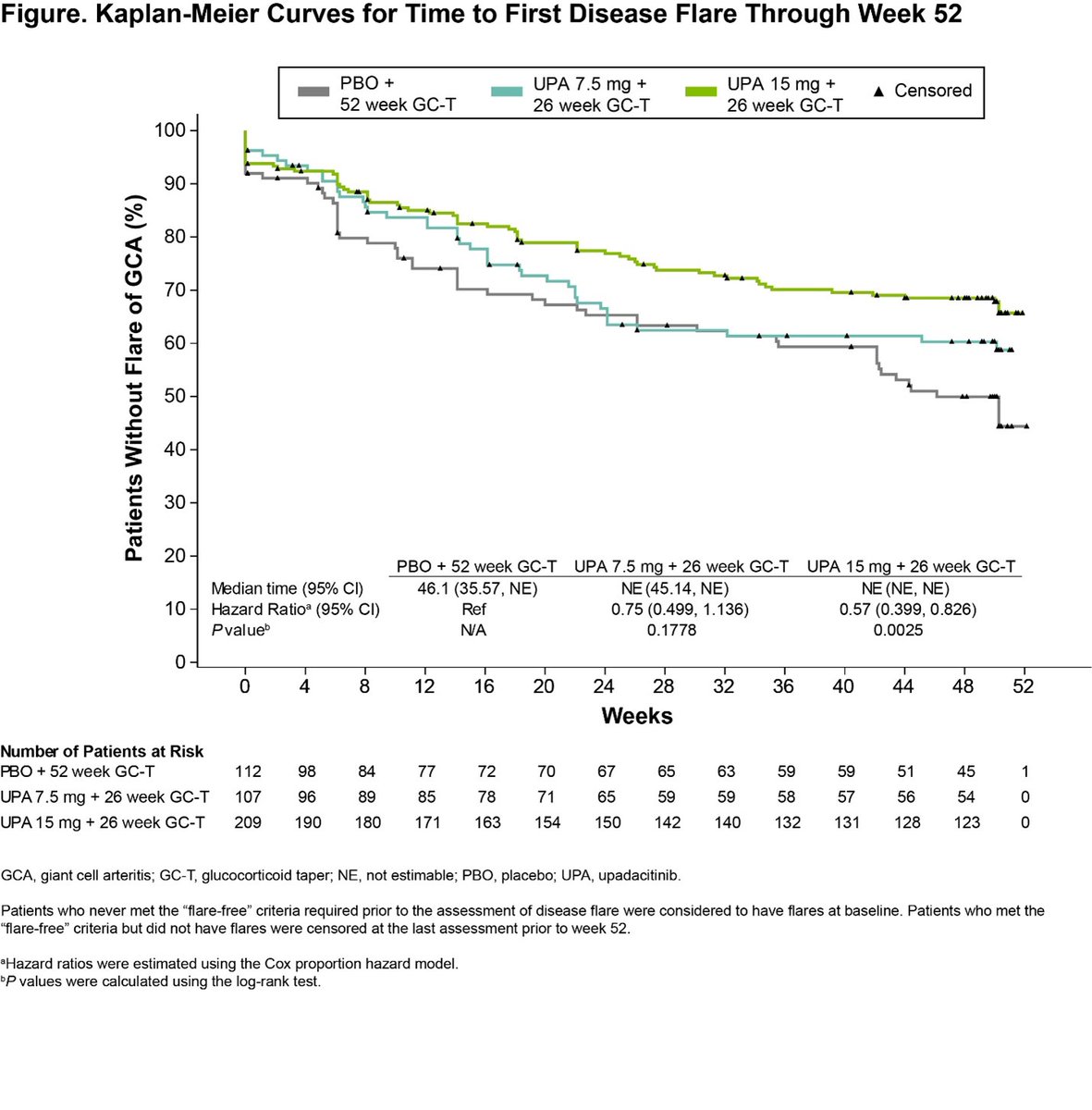
Upadacitinib (UPA), a new oral treatment option for GCA? Dr. Peter Merkel discusses SELECT-GCA.
UPA15 + 26-week GC taper >> PBO with a 52-week GC taper for GCA remission.
#ACR24 #ACRBest @RheumNow ABST#0770 https://t.co/UbQLVA8X7r
Jiha Lee JihaRheum ( View Tweet)

Where do SGLT2i have proven benefits for CVD?
👉 Diabetes w/high CV risk
👉Heart failure (all EF)
👉CKD
Dr Weber @rheumnow #ACR24 https://t.co/vFYddrLP1Y
TheDaoIndex KDAO2011 ( View Tweet)
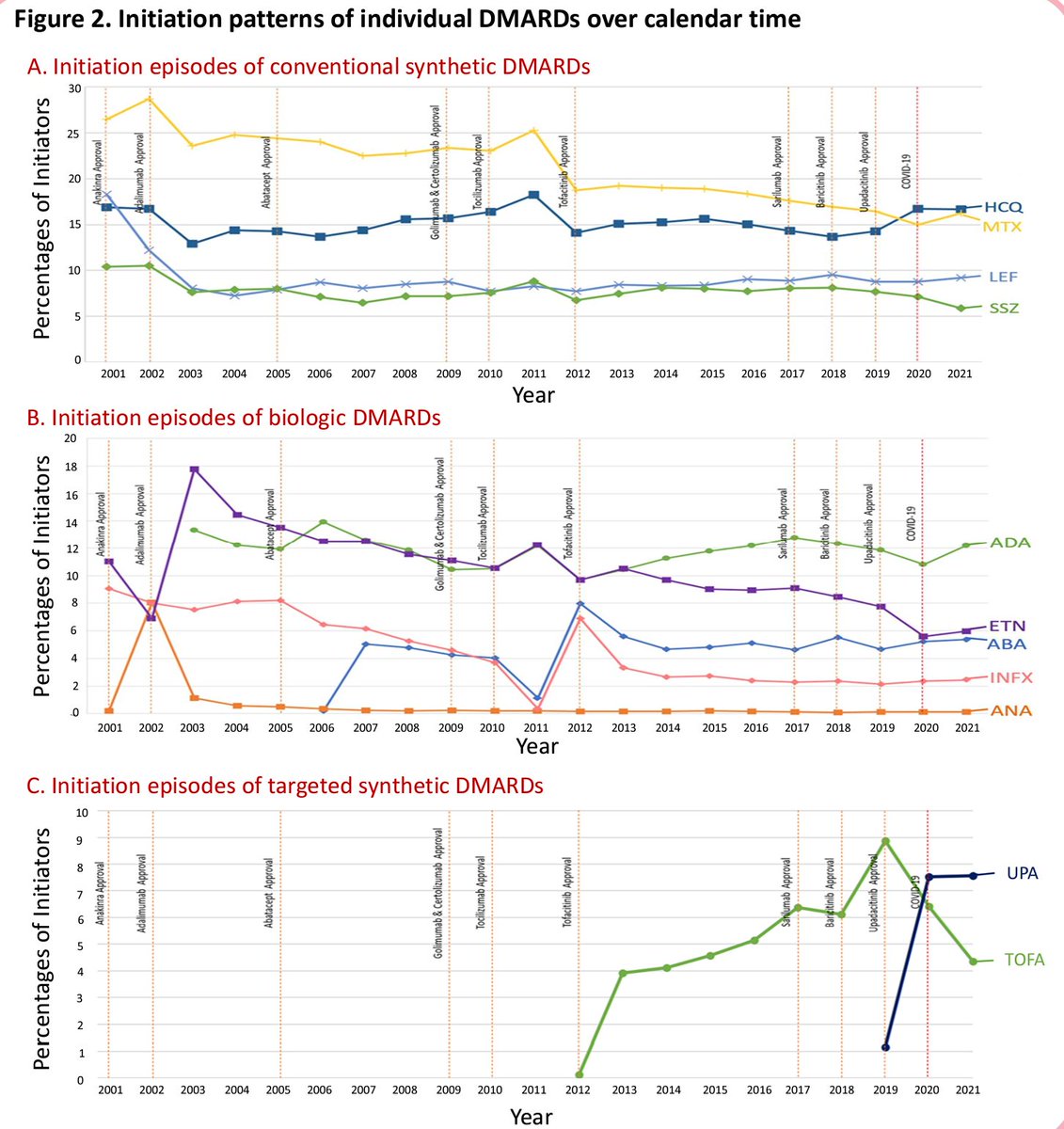
It's been a wild ride over the last 20 years of RA b/tsDMARDs, and fascinating to see how our prescribing habits have changed over that time.
MarketScan data tell a story of fashion and fame. What will the next 20 years be like?
#ACR24 ABST0509 @jeffsparks @RheumNow https://t.co/wCcWgkHrvc
David Liew drdavidliew ( View Tweet)
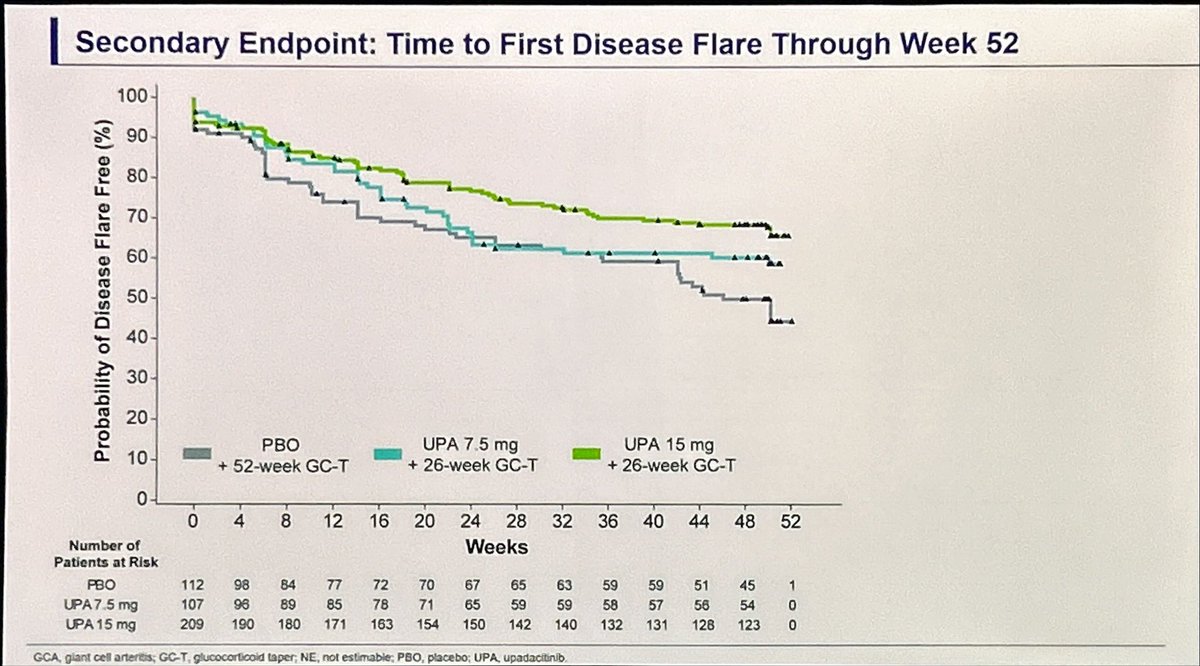
Major update in tx for GCA beyond Toci
SELECT-GCA showed upadacitinib 15mg daily achieving higher rates of remission with SHORTER (26wk) steroid use compared to placebo (52wk)
No significant adverse safety signal w JAKi including MACE/malignancy
@RheumNow #ACR24 Abstract 0770 https://t.co/45D0Txed2N
Links:
Brian Jaros, MD Dr_Brian_MD ( View Tweet)
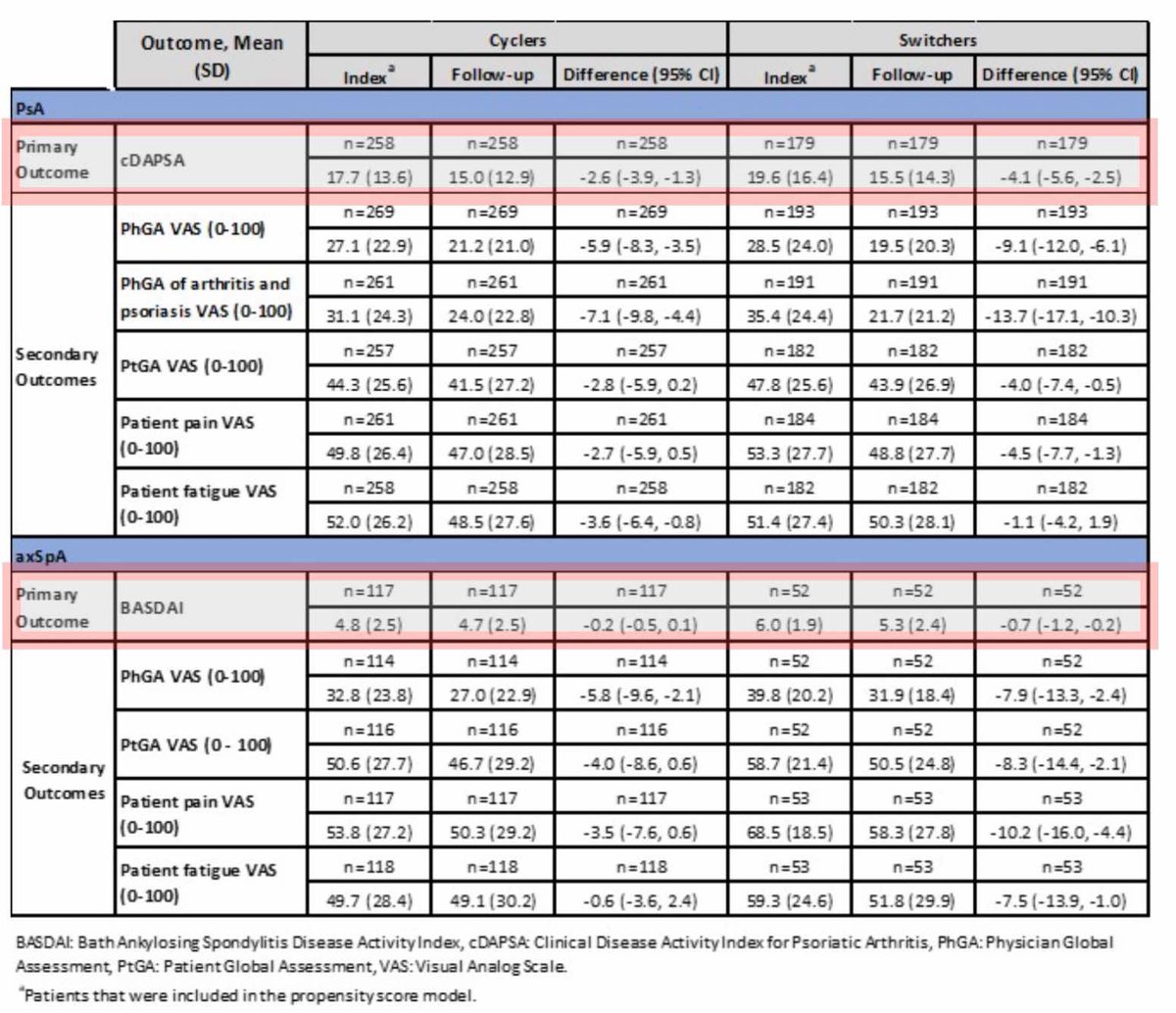
TNFi cycling vs. switching to IL-17Ai?
Dr @AlexisOgdie et al from CorEvitas registry:
PsA & axSpA cohort - switchers (TNFi to IL17i) had greater improvements in cDAPSA & BASDAI vs. cyclers (2nd TNF)
Not stat significant but offers alternative Tx options
@RheumNow #ACR24 abs585 https://t.co/8m347BRM75
sheila RHEUMarampa ( View Tweet)
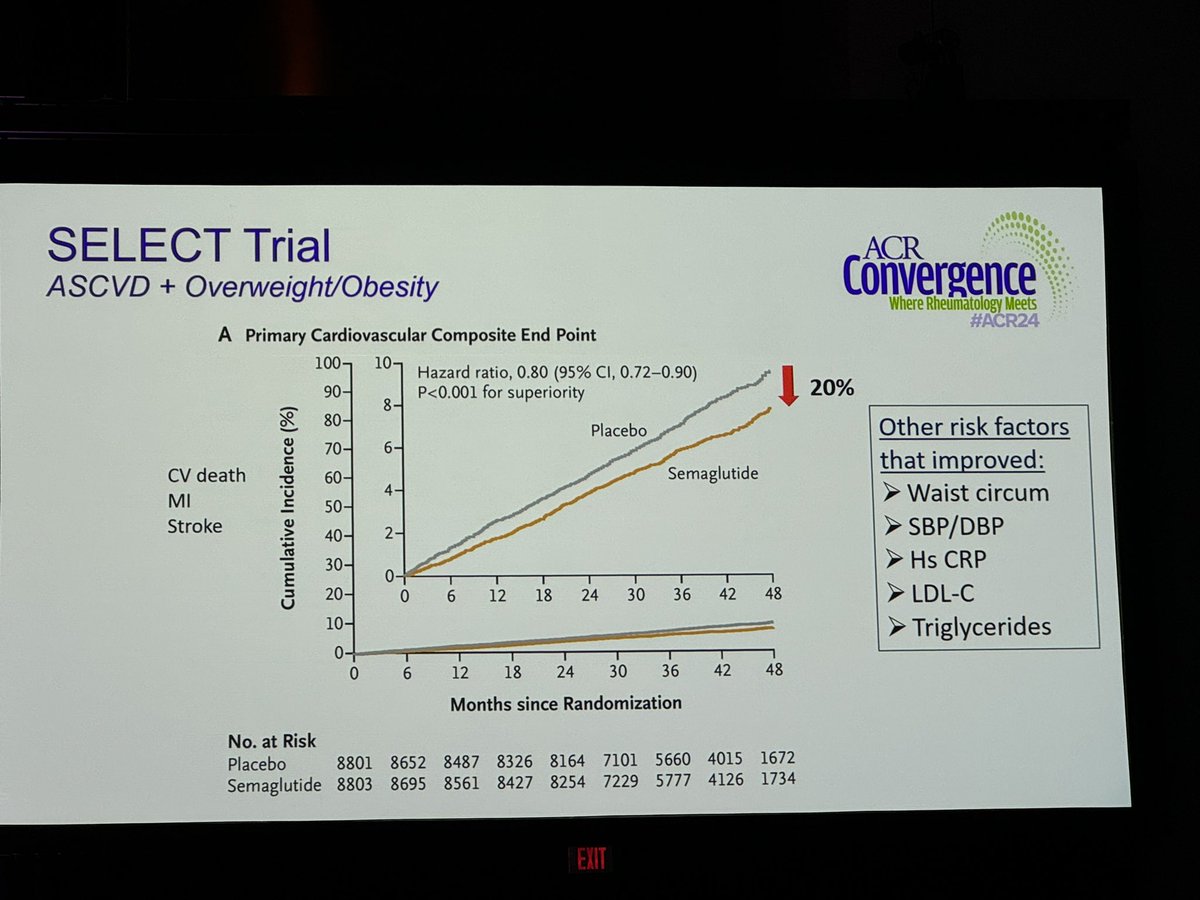
SELECT trial noted reduction in CV death, MI and stroke in obese pts without diabetes (other benefits: reduction in waist circumference, BP, lipids) @rheumnow # ACR24 https://t.co/GPK4Vg5bOt
Links:
TheDaoIndex KDAO2011 ( View Tweet)
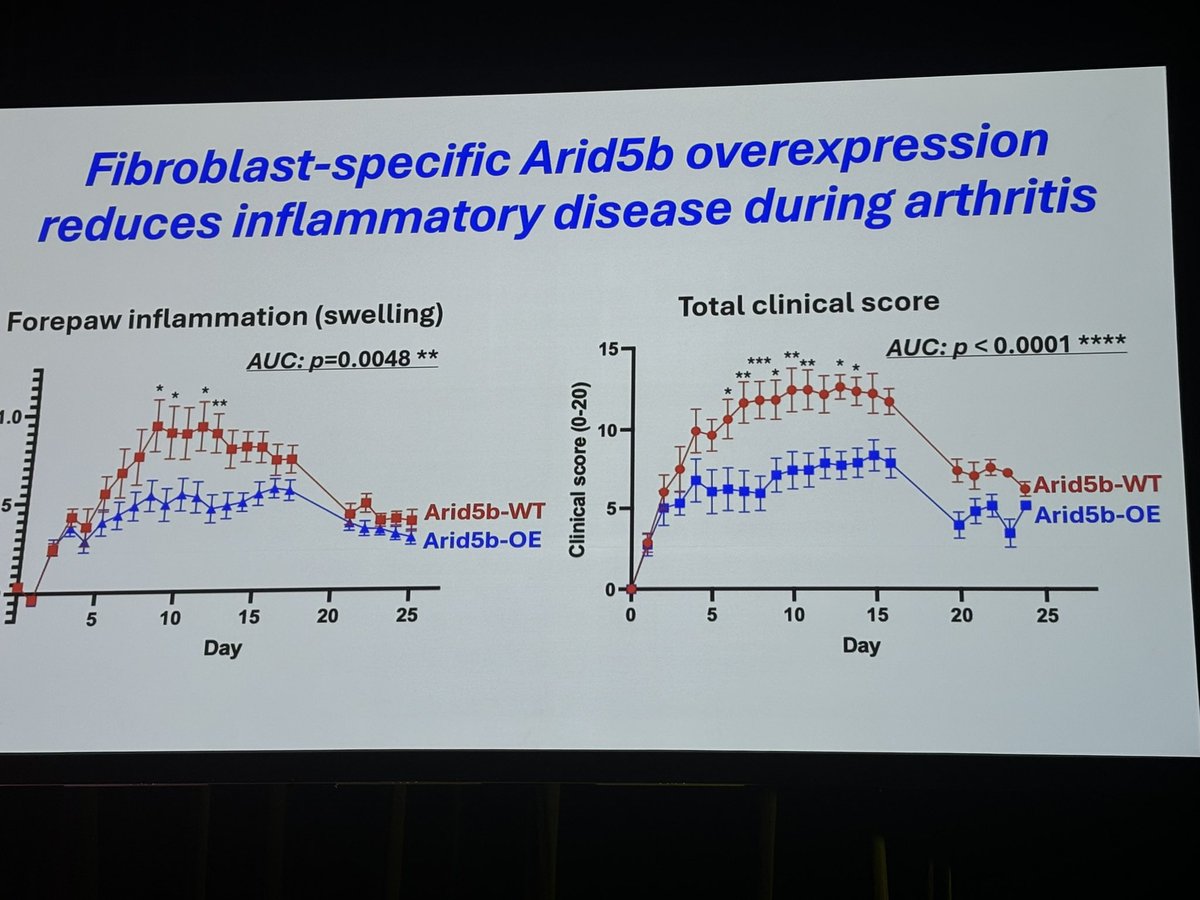
#ACR24 Ab#0771
ARID5B - transcription factor controls pathologic inflammatory fibroblast
ARID5B: RA risk locus on GWAS, also link to SLE, Graves
Binds to histone editors to epigenetically regulate fibroblast state
ARID5B deletion incr inflamm response, overexpr decr
@RheumNow https://t.co/ebKnX1uTuO
Links:
Eric Dein ericdeinmd ( View Tweet)
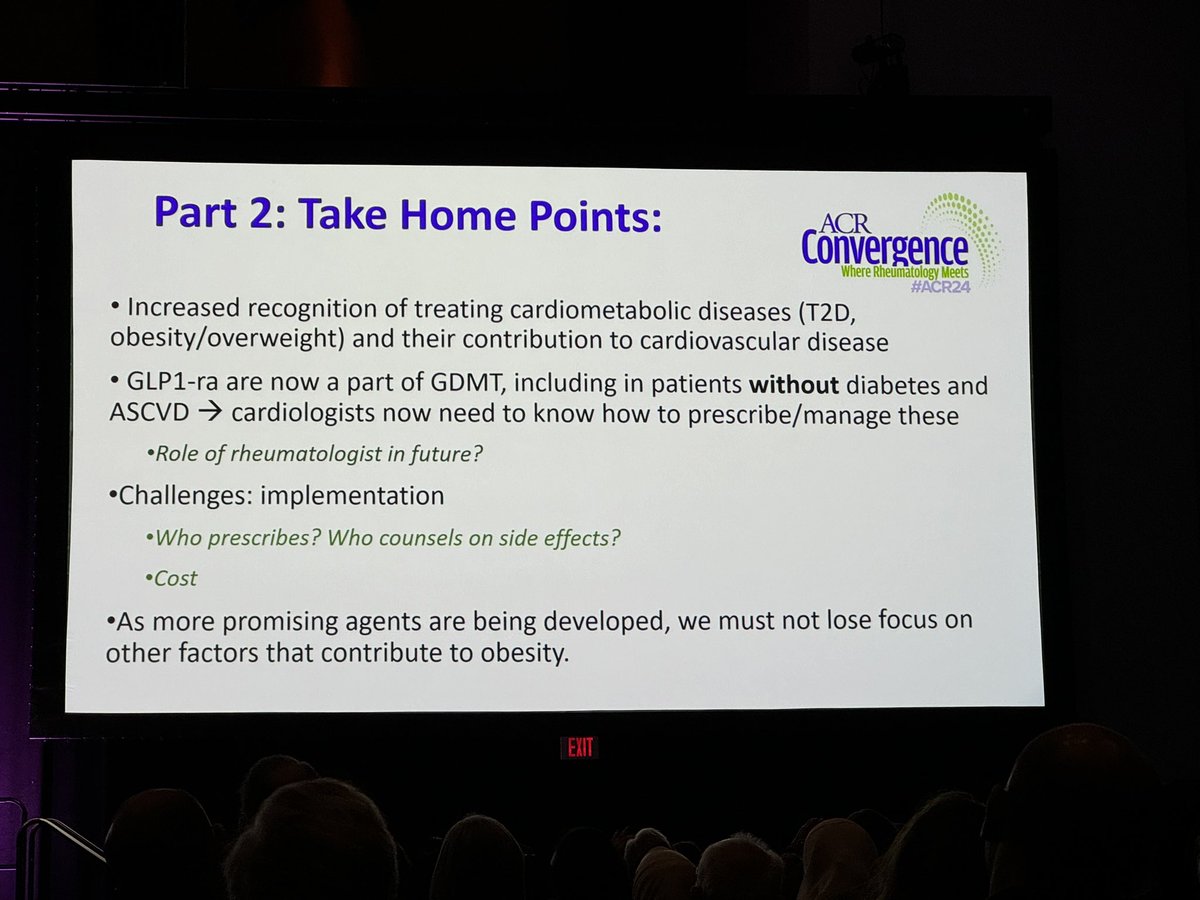
GLP1ra is now part of GDMT, including pts without diabetes. The role of rheums in prescribing these remain to be seen. - Dr Weber #ACR24 @rheumnow @ACRheum https://t.co/U9XEhGBXBN
Links:
TheDaoIndex KDAO2011 ( View Tweet)
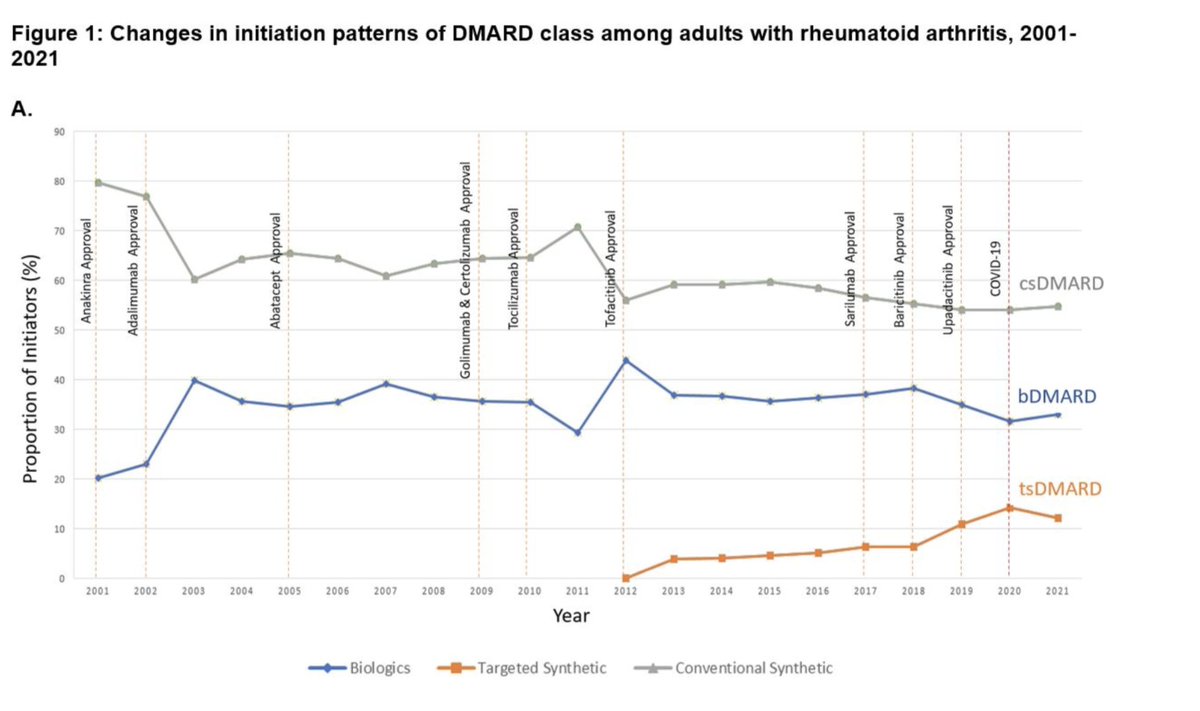
#0509
📊 RA DMARD Trends in US (2001-2021)
🧑🤝🧑 407,728 DMARD starts in 229,365 patients
📉 csDMARD use fell (79.7% → 54.7%)
‼️Methotrexate dropped 29% → 15%
📈 bDMARDs (20.3% →33.1%),tsDMARDs (0.1% → 12.2%) both ⬆️⬆️
💊Biosimilar uptake low
#ACR24 @RheumNow @jeffsparks https://t.co/JepaWj7azY
Caoilfhionn Connolly CaoilfhionnMD ( View Tweet)
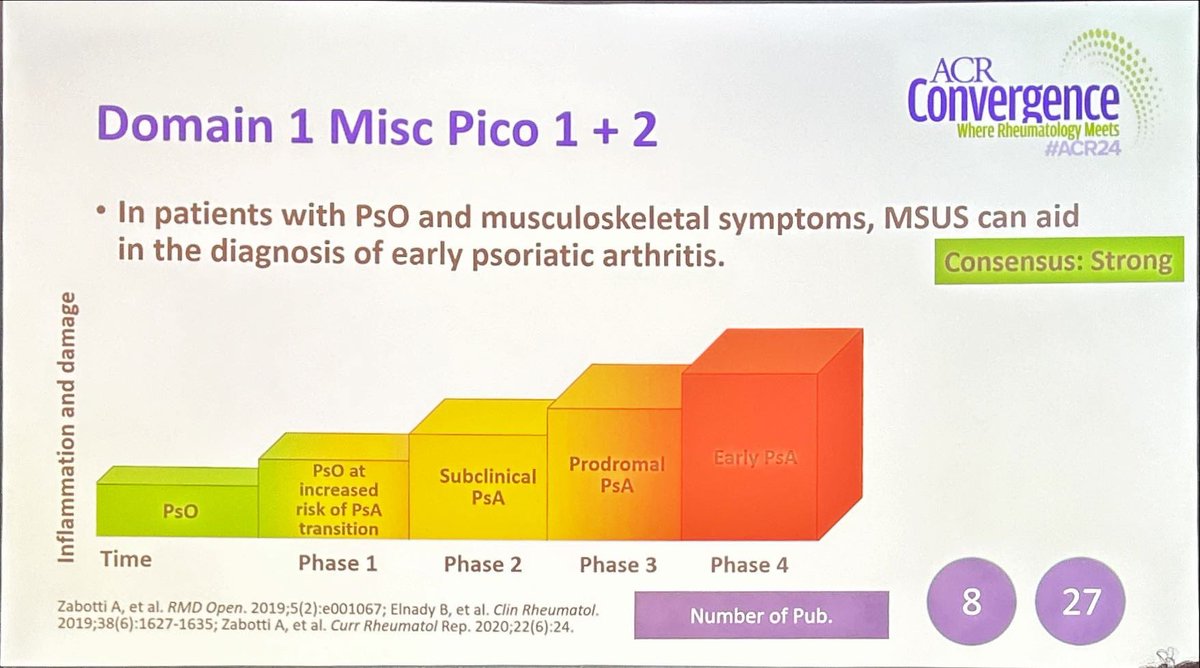
Dr. Catherine Bakewell @CatherineB27 shares the preliminary ACR guidelines on ultrasound imaging in psoriatic arthritis covering 4 domains, detailed PICOs covering the early phase, diagnosis, assessment covering the domains of PsA @RheumNow #ACR24 https://t.co/DoHE1rsSGf
Antoni Chan MD (Prof) synovialjoints ( View Tweet)

#0322🔬 Myocarditis in Myositis(IIM)
📊 26% new IIM pt had myocarditis (ESC,Lake Louise)
💥 Anti-Ku most common MSA
💥Myocarditis a/w ⬆️heart failure, arrhythmia (43 v 6%;p=0.02)
🎯 Myocarditis🟰poor outcomes
🎯Cardiac MRI🟰earlier detection
#ACR24 @RheumNow @JuliePaikMD https://t.co/yz0f2ozFVL
Caoilfhionn Connolly CaoilfhionnMD ( View Tweet)

"If you want an argument, put two rheumatologists in a room and ask them about steroid tapers. Add a third and you'll have a fight"
-P. Merkel at UPA plenary session
#ACR24 @RheumNow
Mike Putman EBRheum ( View Tweet)

How to Master ACR Meetings
https://t.co/ATbOYbatOy https://t.co/j1oRBbhWY2
Dr. John Cush RheumNow ( View Tweet)
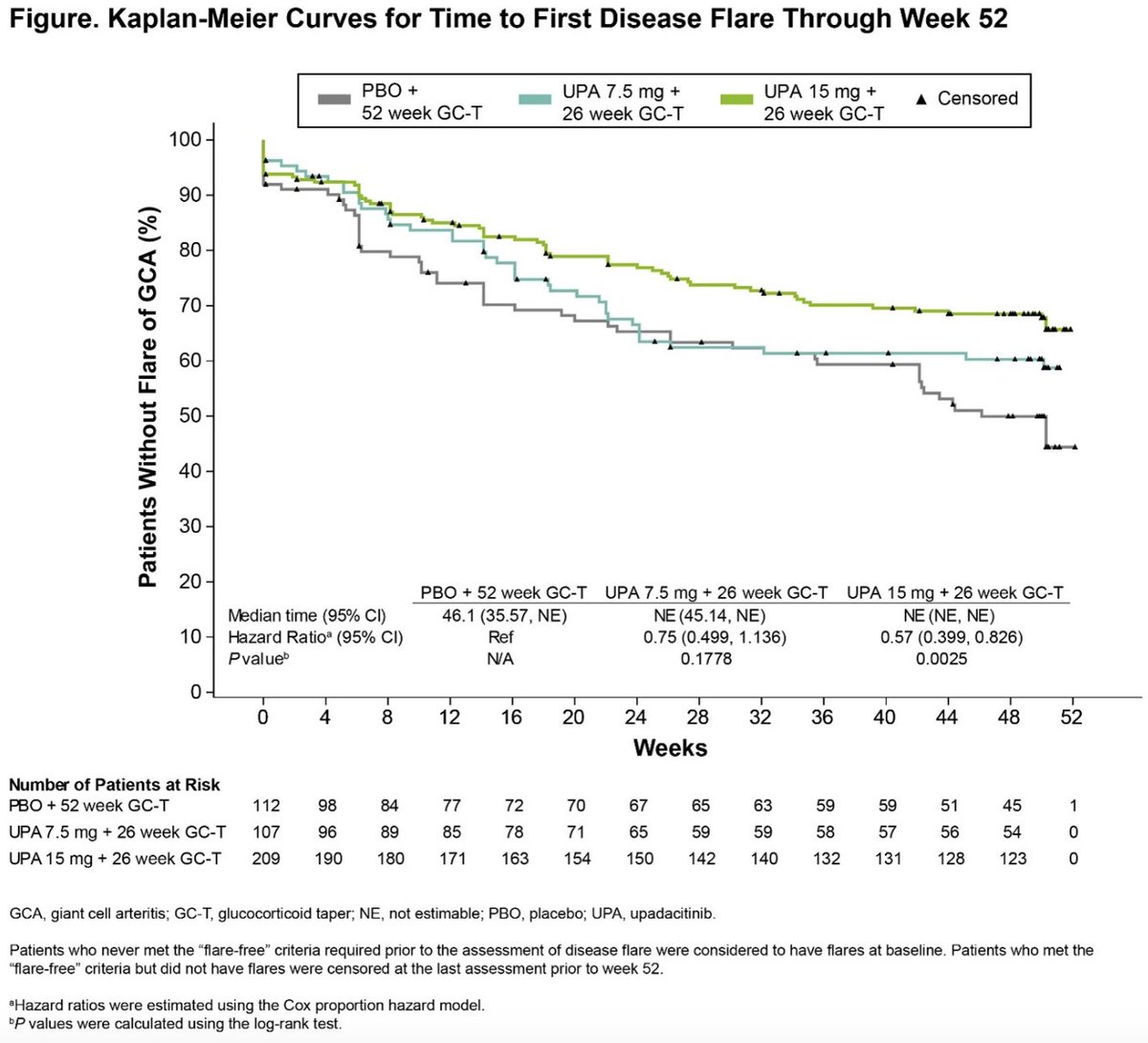
Results from SELECT-GCA ➡️UPA 15mg + 26W GC taper demonstrates superior efficacy & reduced GC use vs PBO + 52W GC taper ➡️No new safety signals Is UPA the new kid on the block in #GCA? Ab0770 #ACRBest #ACR24 @RheumNow https://t.co/pHzozYiid5
Mrinalini Dey DrMiniDey ( View Tweet)
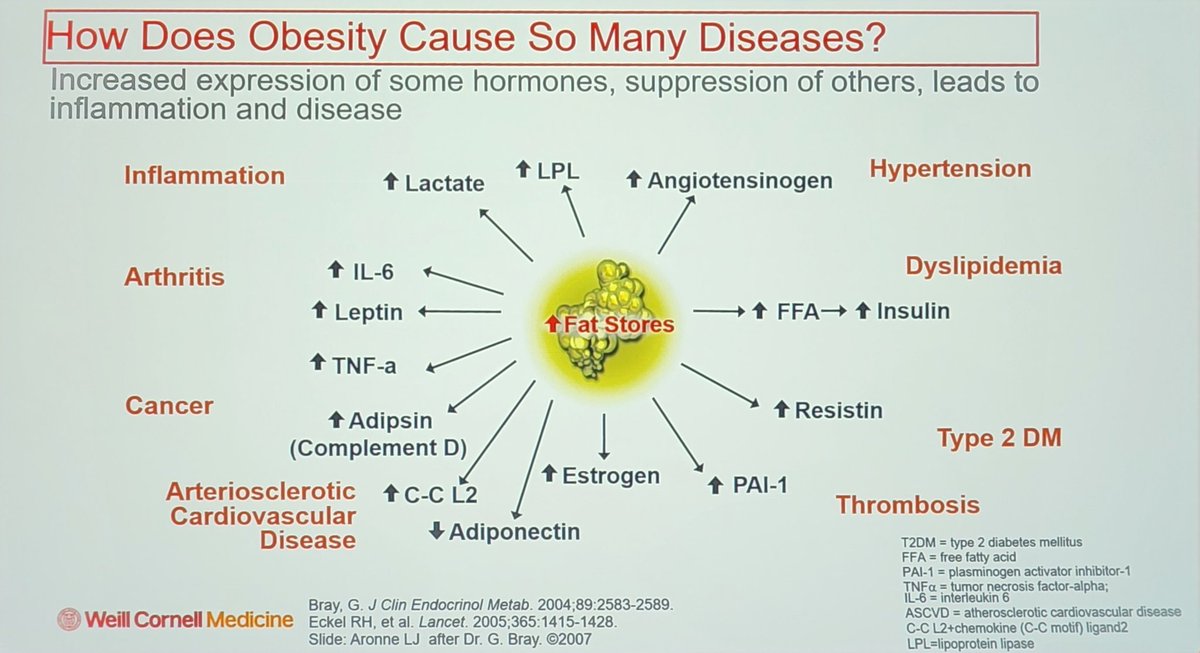
#obesity causes a lot of diseases including #arthritis. How?
⬆️ IL-6
⬆️ leptin
⬆️ TNF-a
@RheumNow #ACR24
@rheumarhyme https://t.co/qeqTZUOEZy
sheila RHEUMarampa ( View Tweet)



