SATISFACTION (2.27.2026)
Dr. Jack Cush reviews the news and journal reports from this past week on RheumNow.com.
Read ArticleDr. Jack Cush reviews the news and journal reports from this past week on RheumNow.com.
Read Article







A report in The Lancet Diabetes & Endocrinology suggested that 3 months of romosozumab (ROMO) followed by denosumab is as effective at increasing hip bone mineral density (BMD) as the standard 12-month course.
Read Article
An economic evaluation of early vs delayed use of the Blys inhibitor, belimumab (BEL), in systemic lupus erythematosus (SLE) has shown both cost effectiveness and clinical utility of early BEL initiation in active lupus patients.
While most would advocate for using your best therapy
Read Article

Currently, fewer than half of patients diagnosed with osteoporosis receive appropriate pharmacologic therapy. This treatment gap reflects several challenges in osteoporosis management, including limited disease awareness, barriers to medication access, clinician discomfort with therapy selection
Read Article
Today Lilly announced top line results of the TOGETHER-PsO open-label, Phase 3b trial demonstrating the significant benefits of concomitant ixekizumab (IXE: an IL-17A inhibitor) and tirzepatide (TIR: GLP-1agonist) over IXE alone.
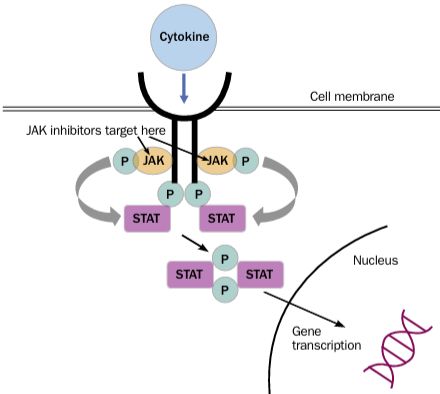
Read ArticleIn 2020, the ACR Recommendations on Reproductive Health notably avoided firm guidance on the use of JAK inhibitors (JAKi) during pregnancy stating, "There is no available evidence regarding use or safety of the new small- molecule agents, tofacitinib, baricitinib, and apremilast, during
Read Article
By downloading this material, I acknowledge that it may be used only for personal use and personal education and that I will accredit RheumNow.com as the source and owner of this material. Commercial use or mass reproduction of this material without permission from RheumNow (info@rheumnow.com) is prohibited.