All News
ACR Best Abstracts - Day 2
Day two at ACR 2022 was full of great sessions on imaging, vasculitis, lupus, vasculitis, spondyloarthritis, COVID, pregnancy, microbiome, economics and more.
Here are the RheumNow faculty selections for #ACRbest abstracts today:
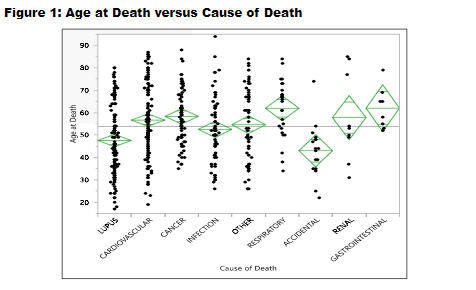
#ACR22 Abstr#2068 Data from John Hopkins showed leading cause of deaths (1985-2019) in #lupus were #SLE & Cardiovascular (both 23%), then cancer & infection.SLE deaths common in younger. African-American died younger vs White. Need to improve with therapies we now have @RheumNow https://t.co/4tDhr1Eodm
Md Yuzaiful Md Yusof Yuz6Yusof ( View Tweet)
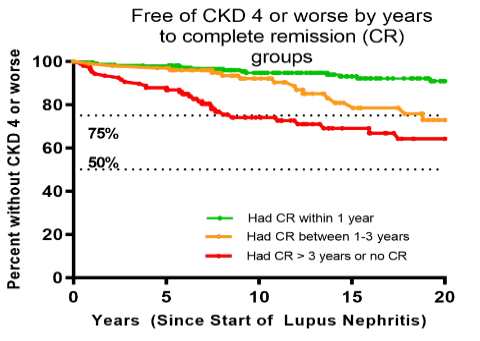
#ACR22 Abstr#2061 It's time to tight control newly diagnosed #lupus nephritis patients. In a cohort study which 16% developed advanced CKD, risk was reduced if remission achieved by 12 mths of diagnosis. =>1 flare & shorter time-on-therapy increased risk
@RheumNow #ACRBest https://t.co/swYn2g4hqe
Md Yuzaiful Md Yusof Yuz6Yusof ( View Tweet)
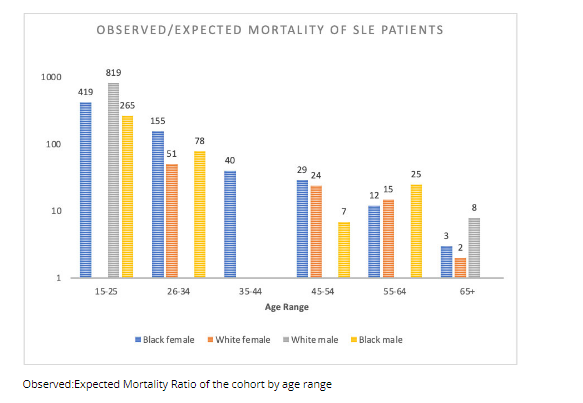
#SLE mortality in South Carolina Lupus Cohort
Standardized mortality ratio (SMR) is higher in blacks
Higher SLICC scores in blacks
abst#2106 #ACR22 @rheumnow https://t.co/NAdNhUHsbc
Bella Mehta bella_mehta ( View Tweet)

New SLE Rx. Deucravitinib a TYK2i phase 2 RCT showed SRI4 endpoint. Subset of 3 mg bid was best vs 6 mg bid and 12 mg OD. Skin via CLASI-50 & other endpoints also positive. Awaiting phase III. Abst1117 #ACR22 @RheumNow https://t.co/fZI3AV5pML
Janet Pope Janetbirdope ( View Tweet)
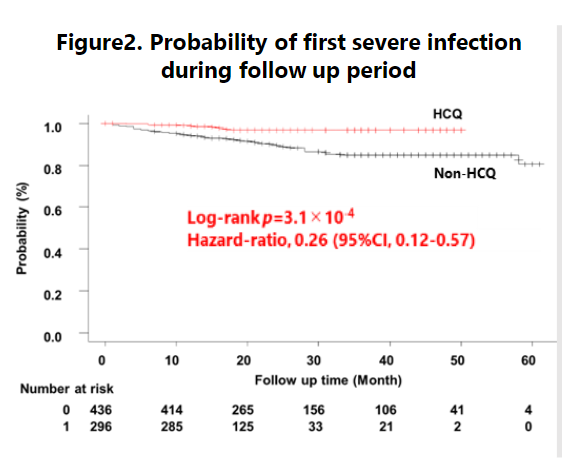
Hidekawa et al. HCQ use assoc reduced severe infection in LUNA SLE registry, HR 0.26. ?due to better disease control rather than anti-infectious role, but HR 0.32 in multivariable model including SLEDAI. @RheumNow #ACR22 Abstr#2059 https://t.co/EgTJOAymoF https://t.co/gmchk9ZS5L
Richard Conway RichardPAConway ( View Tweet)
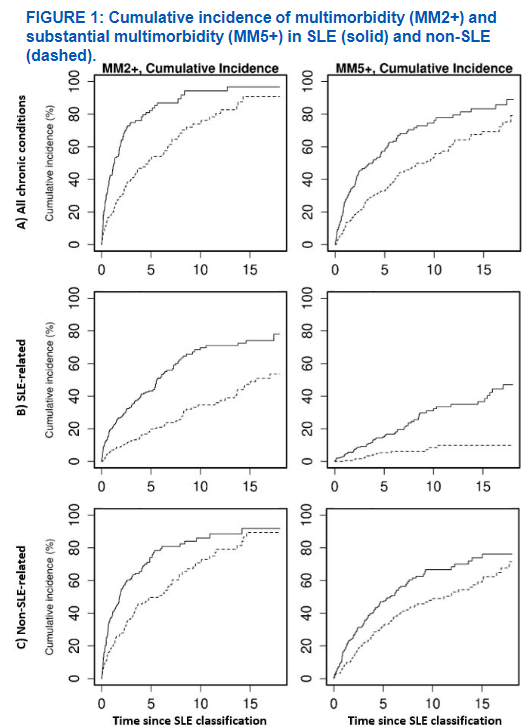
Figueroa Parra @AliDuarteMD et al. Multimorbidity in SLE. Higher at classification - due to non-SLE assoc. SLE-assoc drive increased accumulation over time but non-SLE assoc also increased @RheumNow #ACR22 Abstr#2091 https://t.co/6IyhovSNYA https://t.co/qmYfoqCTtz
Richard Conway RichardPAConway ( View Tweet)
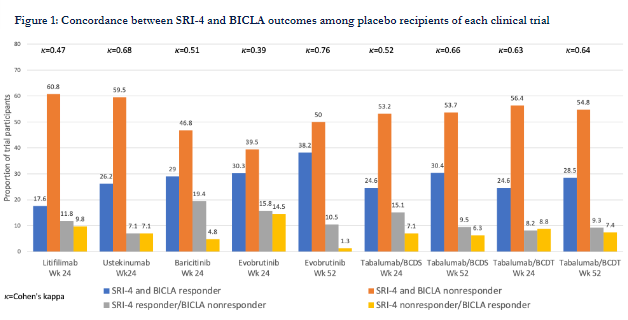
#ACR22 Abstr#2055 SRI-4 and BICLA: how do they converge and diverge? Analyses of 6 x Non-Renal #Lupus RCT showed discordance (12-30%).When discordant, SRI-4 classified more pts as responders vs BICLA. Concordance higher at 52 vs 24 wks. Vital to interpret both outcomes @RheumNow https://t.co/prSfTrv0E8
Md Yuzaiful Md Yusof Yuz6Yusof ( View Tweet)
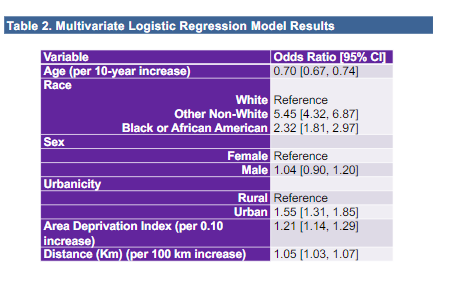
#ACR22 Abstr#1764 In addition to race, what social health aspect to consider when assessing #lupus epidemiology? A study identified urbanicity and area deprivation index were associated with SLE diagnosis. Could those living in the city = better access and diagnosis? @RheumNow https://t.co/PsNt8vQufs
Md Yuzaiful Md Yusof Yuz6Yusof ( View Tweet)
Urine Proteomics in SLE with Dr. Michelle Petri
Dr. Michelle Petri discusses abstract 0536, Change in Urinary Biomarkers at Three Months Predicts 1-year Treatment Response of Lupus Nephritis Better Than Proteinuria, being presented Saturday at #ACR22.
https://t.co/rBDnbSqQCI https://t.co/WfERf1k5VB
Links:
Dr. John Cush RheumNow ( View Tweet)
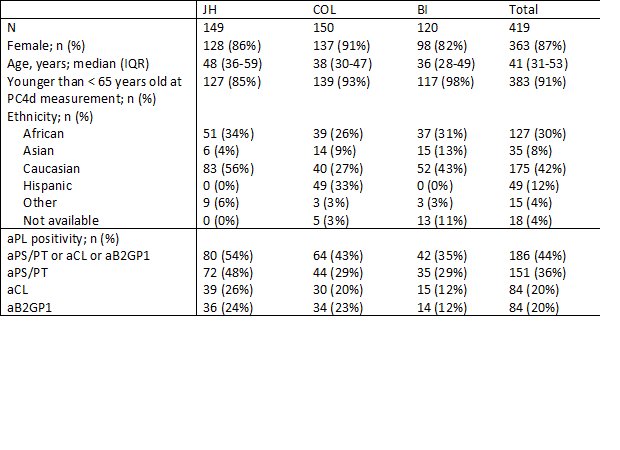
PC4d≥10 MFI is associated with thrombosis in SLE and predicts future arterial thrombosis. Abs 1442 #ACR22 @RheumNow https://t.co/zg7rrOSALs https://t.co/Hs2eOa2vxJ
Dr. Rachel Tate uptoTate ( View Tweet)
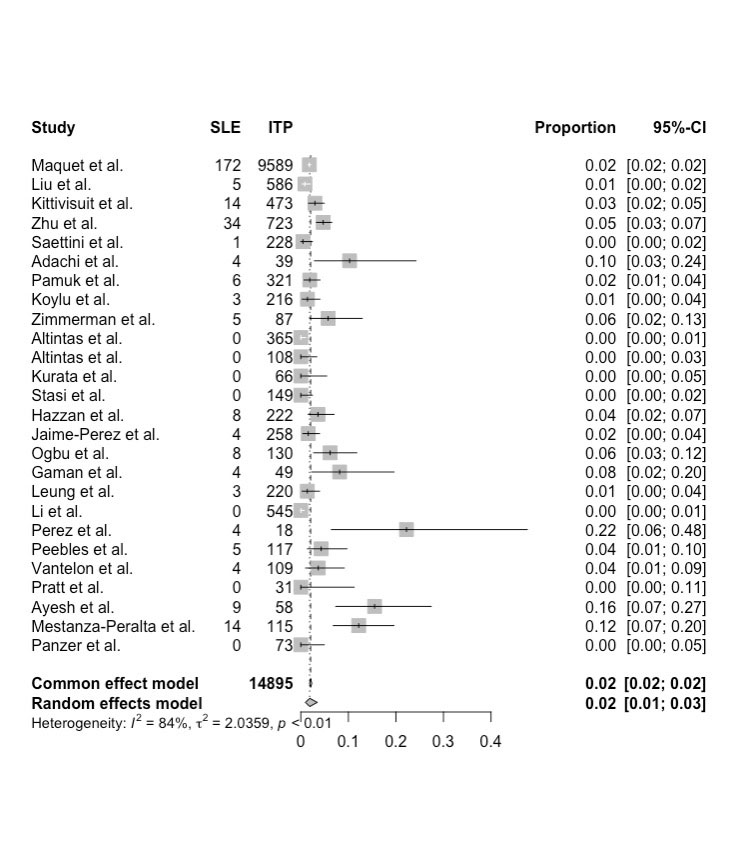
Numerically, SLE was more common in cITP patients. Risks include +ANA and female sex. Abs 1461 #ACR22 @RheumNow https://t.co/0kyqlVphac https://t.co/HfYKCMybdL
Dr. Rachel Tate uptoTate ( View Tweet)
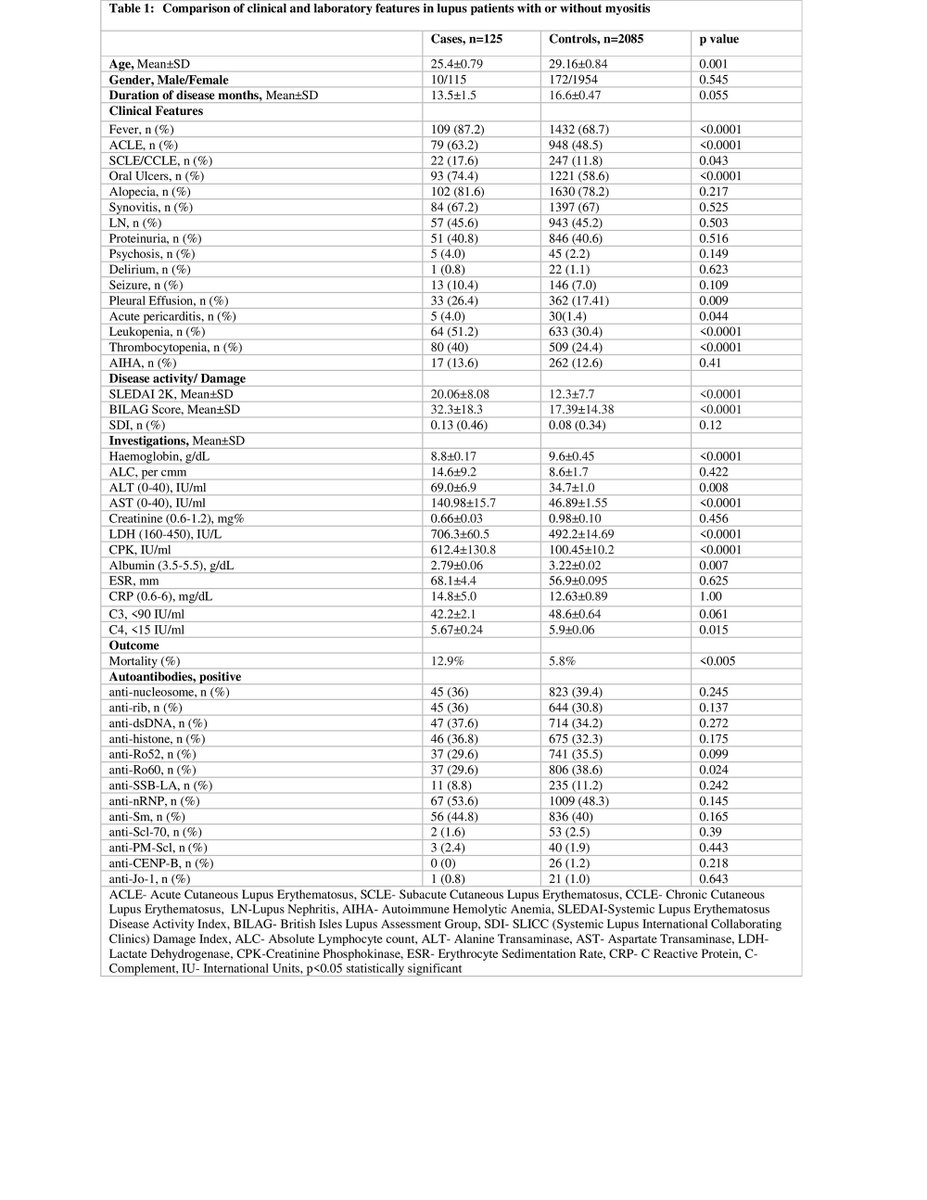
While myositis in the setting of SLE was found to be around 5% in Abs 1453, it was not associated with mortality. #ACR22 @RheumNow https://t.co/hLLuYoXsCv https://t.co/44XGhbPxzW
Dr. Rachel Tate uptoTate ( View Tweet)
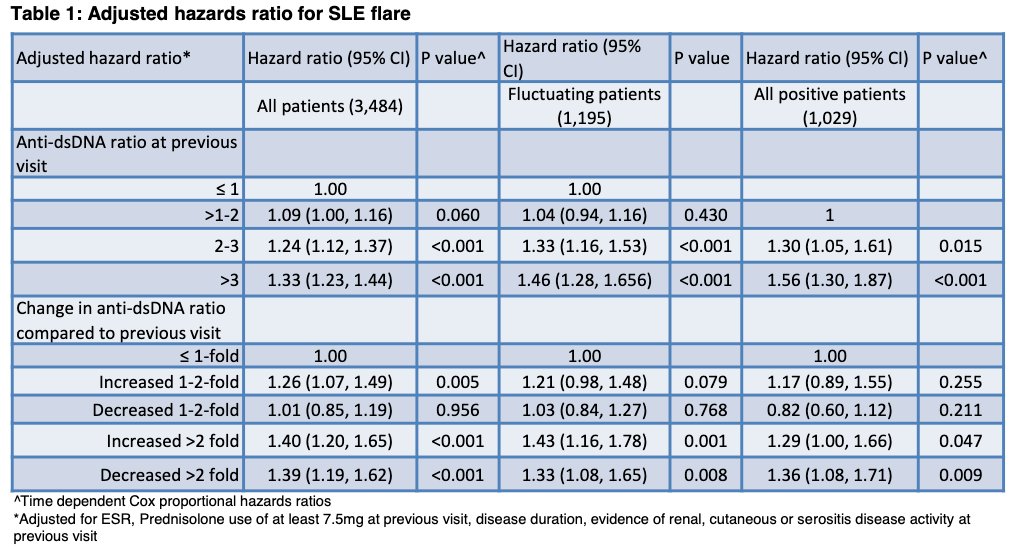
Abst0327 #ACR22 SMART-SLE Monitoring
Some SLE patients with +dsDNA have persistent positivity, others have fluctuations
Anti-dsDNA in persistently positive HR 1.56 for flare risk
Change (up or down!) in dsDNA more than 2x prior visit for fluctuating patients: HR 1.43
@RheumNow https://t.co/YwDPTYWPLu
Eric Dein ericdeinmd ( View Tweet)
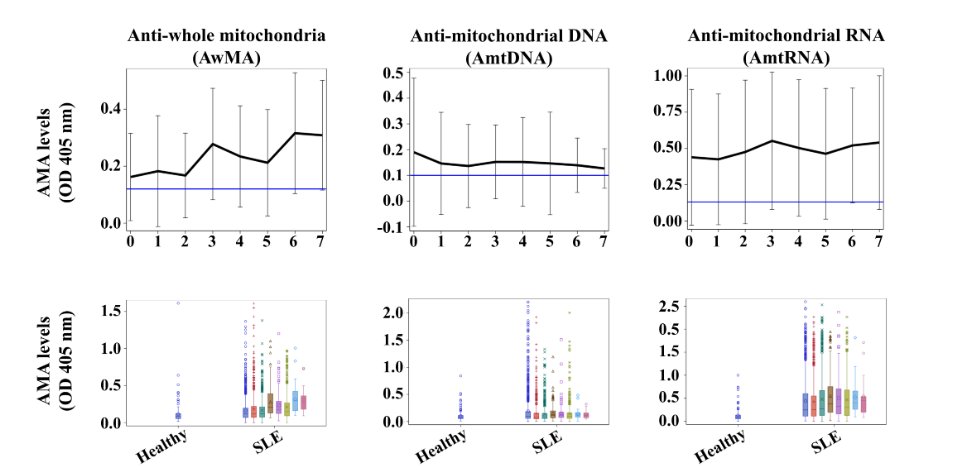
Abst0326 #ACR22 Anti-Mitochondrial Ab in SLE
Whole mitochondrial (AwMA), AmtDNA or AmtRNA - higher in SLE compared to controls
AwMA predictive of death, AmtDNA and AmtRNA predictive of nephritis
@Rheumnow https://t.co/d98HSHnJVE
Eric Dein ericdeinmd ( View Tweet)
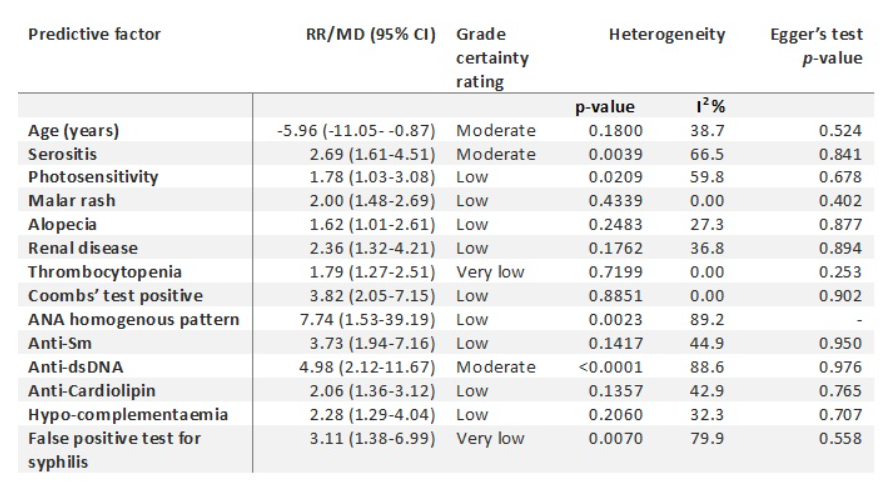
Abst0328 #ACR22. Predicting UCTD to CTD Meta-Analysis
Factors for SLE transition: younger age, serositis, dsDNA
SSc transition: puffy finger, NFC, or SSc antibodies
No studies wo moderate or high risk of bias
Limited studies on biomarkers for SLE, need more studies
@Rheumnow https://t.co/GofGF8TkCx
Eric Dein ericdeinmd ( View Tweet)
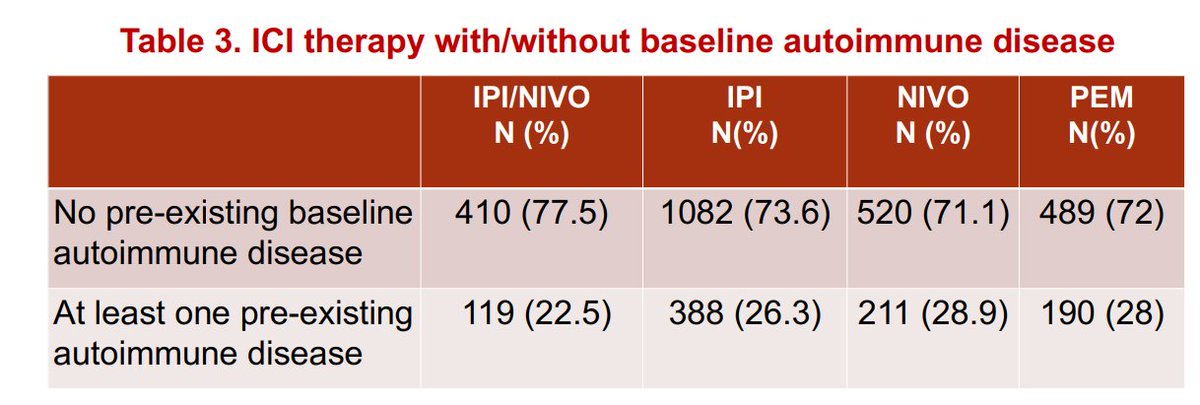
Is channelling bias a risk, because of treating clinicians 'protecting' pre-existing autoimmune dx pts: maybe?
Certainly in practice, these pts might get less combo immunoRx; this @mcgillu data would suggest so
Much more to understand across tumor streams
ABST0760 #ACR22 https://t.co/z1rhAJZ9gj
David Liew drdavidliew ( View Tweet)
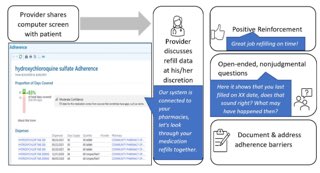
Only 4 minutes to discuss adherence in #SLE. Implementation of discussion if <80% of meds filled. Academic docs - 20/24 used + reinforcement, validated in 17 Pts, 11/24 asked open ended ?s. Pts thought it was right timing. ?does it change behaviour- ? Abst0063 @RheumNow #ACR22 https://t.co/UQbRgw5Emj
Janet Pope Janetbirdope ( View Tweet)
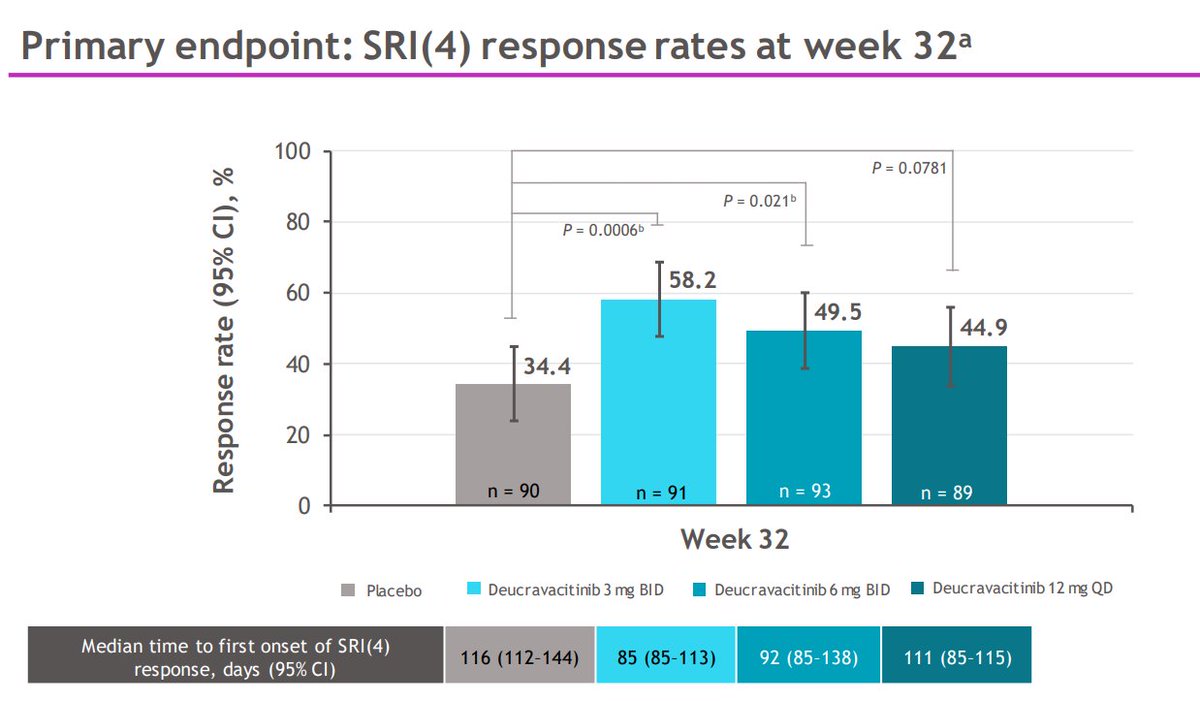
Pike et al. Deucravactinib (TYK2i) in SLE. + on SRI(4) week 32. + SRI(4),BICLA, LLDAS, CLASI-50, swollen and tender joint counts week 48. Strange, the lowest dose (3mg bd) seems best. @RheumNow #ACR22 Abstr#1117 #ACRbest https://t.co/o4902tvZs8 https://t.co/t8oeMRGUS7
Richard Conway RichardPAConway ( View Tweet)
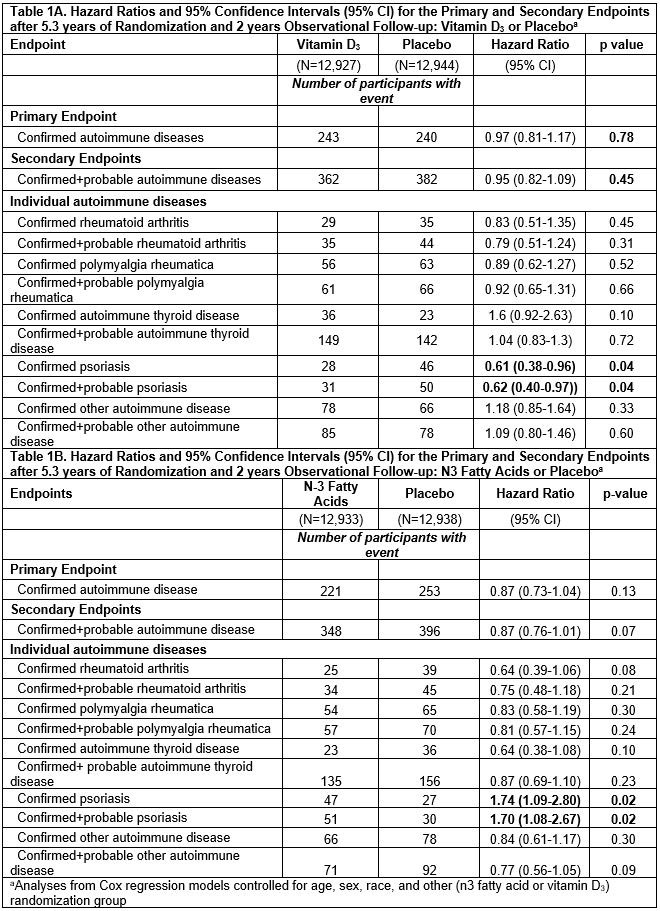
2000 IU/day vitamin D led to significantly reduced incidence of autoimmune diseases in Abs 1200 over 5.3 years, but after trial termination, protective effects dissipated and were no longer significant. #ACR22 @RheumNow https://t.co/sLwoxeCR3y https://t.co/47wpWXF1W7
Dr. Rachel Tate uptoTate ( View Tweet)




