Vasculitis Pearls Save

Once again RheumNow Live 2024 really delivered with high impact learning packed into short sessions. As someone with an interest in vasculitis it was fantastic to see four of my favorite speakers in the Vasculitis Mavens and STEP talks. They gave us what we really want from these talks – personal opinions and approaches that go beyond the guidelines. They really dropped a selection of pearls on us and I wanted to share a few of these with you.
Dr. Philip Seo covered GCA and EGPA. It was his approach to GCA that challenged my own practice and made us think again about things.
For new onset GCA he generally uses tocilizumab. This matches my practice, but many people are still stuck in the steroid monotherapy first and tocilizumab if relapses paradigm. Sometimes this is enforced by regulatory agencies, but many rheumatologists continue to think it is best practice also. This is crazy to me, tocilizumab for GCA has been proven as one of our most effective treatments for any rheumatic disease in GiACTA and we continue to treat these patients with one of our most toxic treatments – high dose glucocorticoid monotherapy. None of us would think of treating rheumatoid arthritis without using a DMARD, so why do we do it in GCA?
The second high value piece was his approach to maintenance in tocilizumab treated patients. He generally continues tocilizumab in those with relapsing disease, visual issues, or who want to continue – this matches my practice exactly. It is in the other patients where we do things differently. I guess I am quite conservative – I usually do weekly tocilizumab for the first year and then switch to every second week tocilizumab and continue that long-term if it maintains remission. Dr. Seo describes an approach to increase dosing interval even further to every 4 weeks and then ultimately stop. This is intriguing and I don’t think we have the data to support either approach at present. It will be interesting to see emerging research in this area over the next few years as we build up experience with tocilizumab in GCA.
Drs. Anisha Dua and Mike Putman covered GPA management in 2024.
Again there were some excellent pearls here based on both reinforcement of very clear data which some rheumatologists seem determined to ignore and on personal nuance and opinion. The first was around glucocorticoid tapering in GPA. It is actually surprisingly refreshing in many ways how enthusiastically rheumatologists have embraced the lower dose glucocorticoid taper from the PEXIVAS trial and implemented this in clinical practice. Both speakers emphasised the key point however that the PEXIVAS low dose regime worked on average, there are important caveats around inclusion criteria and the consideration of the individual patient sitting in front of you in choosing glucocorticoid regime. The PEXIVAS low dose taper is correct for many people – it may not be sufficient for some as an initial plan and certainly if people relapse on it the taper needs to be revised. There also are a cohort of patients who likely need even less glucocorticoids then this regime provides.
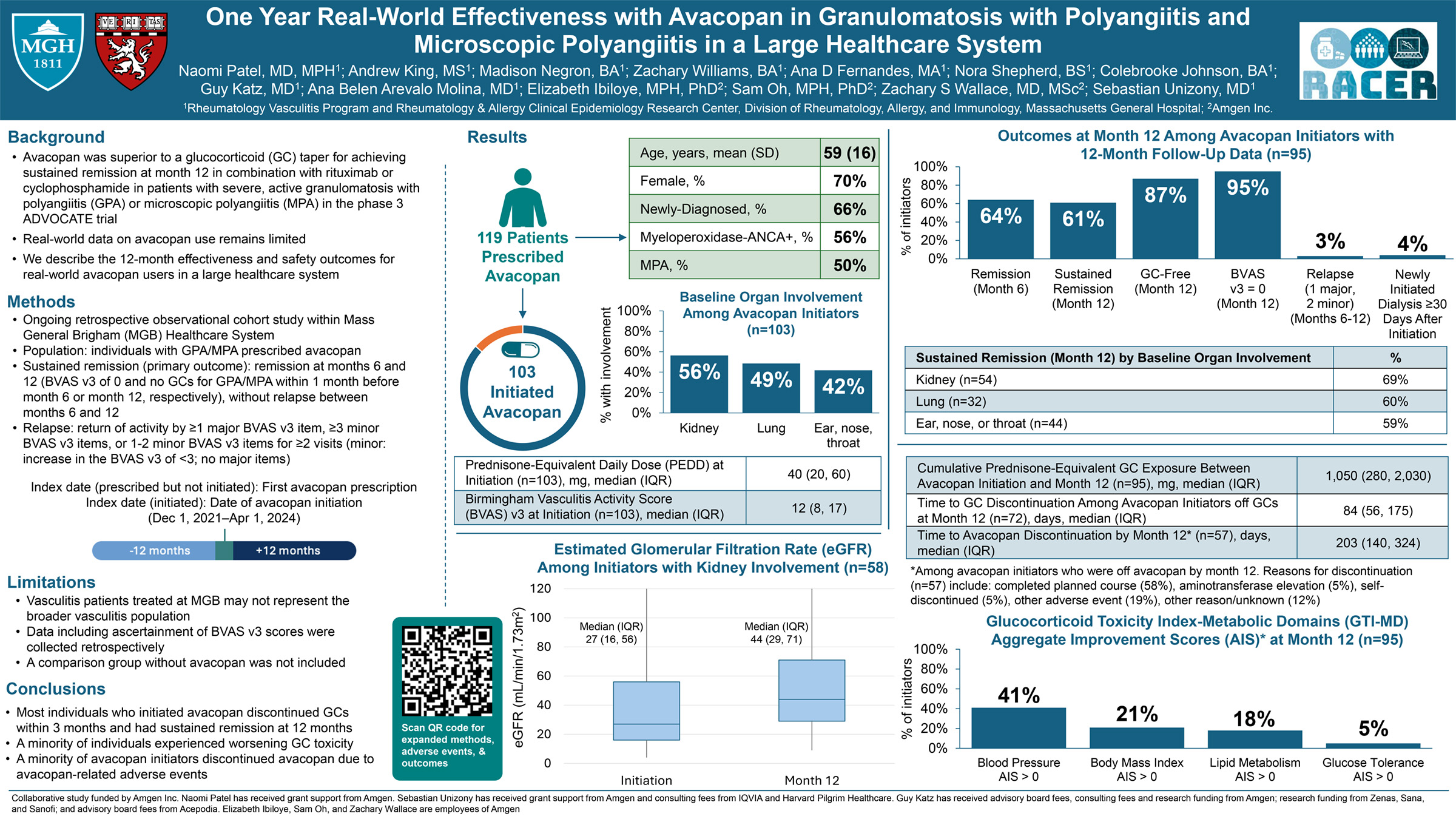
There was then an excellent summary of the MAINRITSAN trial programme results – these have clearly shown that 1) Rituximab is the optimum remission maintenance treatment in GPA, 2) Rituximab should be at fixed 6-monthly intervals for the first 2 years, 3) Rituximab should continue longer than 2 years, 4) if using a retreatment strategy based on labs rather than fixed 6-monthly dosing, then monitoring B-cell repopulation is superior to ANCA return or titre. There remain many unclear issues in GPA however, 1) What dose of Rituximab is best, trials have used both 500mg every 6 months or 1000mg every 4 months – this is a big difference in dosing!, 2) after 2 years do we continue 6-monthly Rituximab or switch to a B-cell repopulation approach, or maybe switch to fixed 12-monthly dosing?, 3) How do we use Avacopan and how would the data look if it was compared to standard of care rather than suboptimal rituximab? 4) Should we treat severe diffuse alveolar haemorrhage with plasma exchange?
The recent improvements and clarity in vasculitis management are heartening but there are still many important unanswered questions for us to work on over the next few years. Until then, we could do far worse than listening to the experts who presented to us at RheumNow Live 2024.










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.