Vasculitis
Sunday’s vasculitis session at RNL26 was a fantastic update on inflamed blood vessels, large and small, by two experts in the field: rheumatologist Dr. Mike Putman and dermatopathologist Dr. Clay Cockerell.
Read Article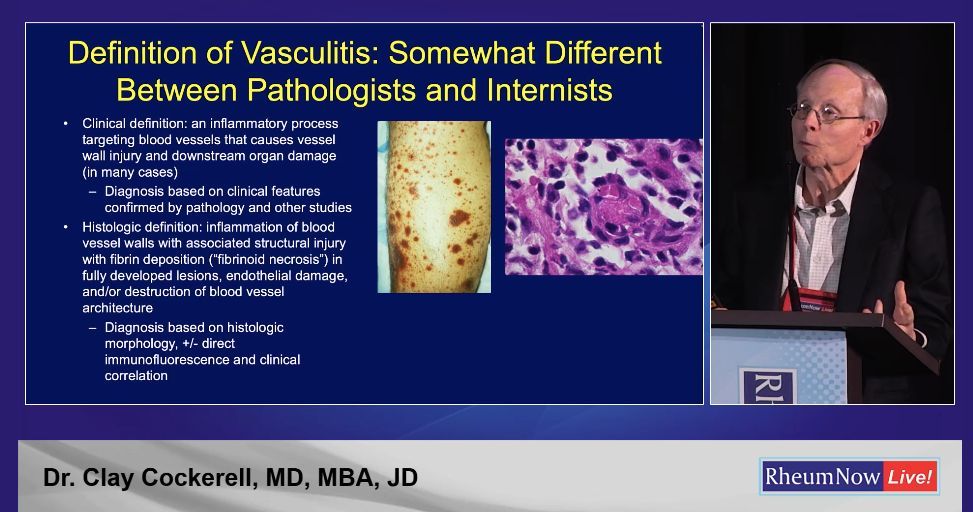
Links:
Sunday’s vasculitis session at RNL26 was a fantastic update on inflamed blood vessels, large and small, by two experts in the field: rheumatologist Dr. Mike Putman and dermatopathologist Dr. Clay Cockerell.
Read Article
Dr. Jack Cush reviews the news, journal articles and regulatory news from this past week on RheumNow.com
Read ArticleThe FDA has requested that Amgen voluntarily withdraw avacopan (Tavneos), a treatment for anti-neutrophil cytoplasmic autoantibody (ANCA)-associated vasculitis, but the company said it has no plans to pull the drug from the market.
Originally developed by ChemoCentryx, the oral
Read ArticleA retrospective cohort study of patients with giant cell arteritis (GCA) demonstrates relapses are common and seen in nearly half of patients, were common after treatment is stopped and is not effectively averted by methotrexate (MTX).
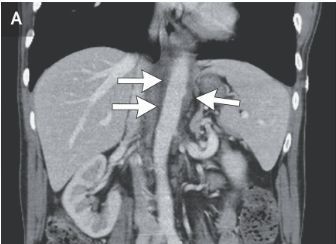
Read ArticleThe The Tocilizumab in Giant Cell Arteritis Spanish Collaborative Group studied giant cell arteritis with aortitis, comparing the efficacy of intravenous vs. subcutaneously (SC) tocilizumab (TCZ) - demonstrating the superiority of SC TCZ.
Read ArticleDr. Jack Cush reviews the news and reports from the past two weeks on RheumNow.Com
Read Article


Dejaco and colleagues have published a glossary of terms often used in conjunction with giant cell arteritis. The glossary of definitions for 23 signs and symptoms of GCA was developed through a consensus process involving international experts.
Read ArticleA current systematic review in Rheumatology addresses the clinical features seen in the VEXAS syndrome.
Read ArticleDr. Jack Cush reviews the news, journal and regulatory reports from this past week on RheumNow.com. B cell drugs in SLE and ITP, biomarkers in GCA & PSS and great videos by APPs.
Read Article
Links:

Links:
Dr. Jack Cush reviews the news and journal reports from this past week on RheumNow.com.
Read ArticleA review of patient data from the International AutoInflammatory Disease Alliance (AIDA) Network registry identifying those with mucocutaneous Behçet’s disease (BD) may progres to major organ involvement (MOI)m especially at later stages.
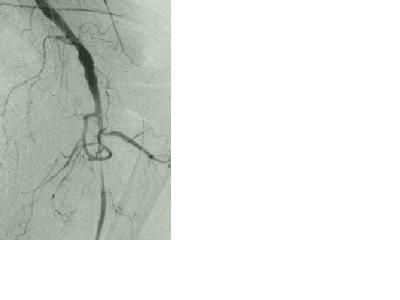
Read ArticleGiant cell arteritis (GCA) is the most common form of adult vasculitis in the United States and can be subdivided into those with cranial only symptoms, those with large vessel vasculiti/PMR, and those with mixed features. Non-invasive imaging is key in detecting large vessel
Read ArticleDrs. Jack Cush & Arthur Kavanaugh, two of rheumatology’s most trusted voices, provide a breakdown of the latest breakthroughs and hottest topics in rheumatology from the 2025 ACR Convergence meeting in Chicago.
Read ArticleThey say the easiest bit about GCA, like PMR, is the first week after you start steroids. Those fond memories belie the challenge of ongoing treatment in GCA. In a steroid-only world, there is only misery. Steroid-sparing therapies have changed this completely.
Read Article
Mrinalini Dey @DrMiniDey( View Tweet )
By downloading this material, I acknowledge that it may be used only for personal use and personal education and that I will accredit RheumNow.com as the source and owner of this material. Commercial use or mass reproduction of this material without permission from RheumNow (info@rheumnow.com) is prohibited.