All News
Late-Onset Disease: Different Age, Different Rules?
We’re seeing more patients develop rheumatic diseases for the first time in their 60s, 70s, or beyond. But are these truly the same diseases we see in younger adults, or do they behave differently, shaped by age-related biology, comorbidity, and the biases that influence medical decision-making? Several abstracts presented at EULAR 2025 challenge us to reconsider how we diagnose and treat rheumatic disease in older adults.
Read Article2025 EULAR/ACR Risk Stratification Criteria for At-Risk Arthralgia
A collaborative EULAR/ACR expert panel has established criteria for arthralgia patients at risk (clinically suspect arthralgia) to progress to chronic rheumatoid arthritis (RA).
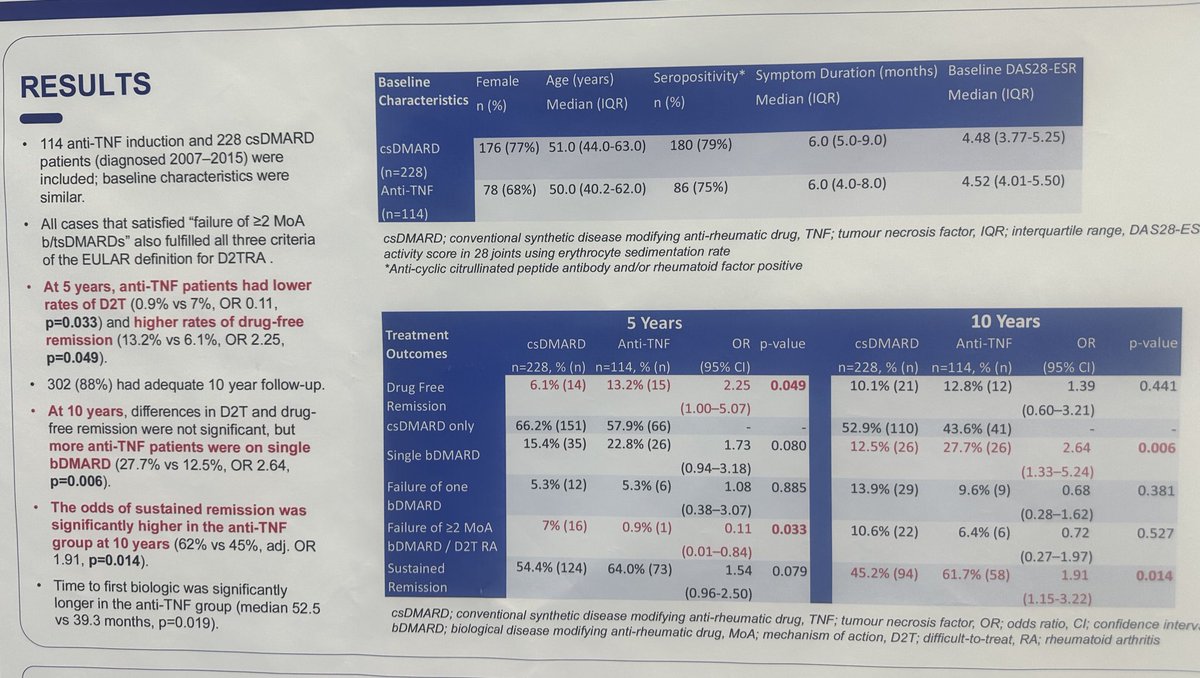
First line TNFi in RA in 140+ pts vs Standard of Care
At 5 yrs outcome
OR drug free remission 2.2
But no longer significant at 10yrs
OR sustained remission 10yrs 1.91
OR single bioDMARDs 10yrs 2.64
Less 1% D2T
#Poster0027 #EULAR2025 @RheumNow https://t.co/sL2XCbxPbl
Aurelie Najm AurelieRheumo ( View Tweet)

Comparative efficacy of tofacitinib vs. adalimumab in RA - metanalysis of 9 RCTs, 24,643 pts finds Tofa signif superior to ADA for ACR20 (RR 1.28), HAQ-DI, VAS, but no difference in adverse events (RR 0.96) or DAS28-CRP improvement https://t.co/5mVY2Qvdms https://t.co/czxnlYHEAl
Dr. John Cush RheumNow ( View Tweet)

Ph 2 open label RCT TOFA in RA-ILD 52 wks
39pts 92% AE 8% 3 deaths FVC decline -69 ml
No diff between UIP, NSIP or antifibrotic
No control group
#POS0619 #EULAR2025 @RheumNow https://t.co/3lqEUfObG9
Aurelie Najm AurelieRheumo ( View Tweet)

Early PsA? Treat fast, treat hard.
The STAMP RCT showed that early secukinumab + MTX led to faster ACR50 and PASI90 responses vs standard care in a T2T strategy. By 12 months, outcomes were similar, but early SEC needed fewer escalations.
Abstract#OP0092
@RheumNow #EULAR2025 https://t.co/cAZTc9eN16
Jiha Lee JihaRheum ( View Tweet)

#OP0066 Danish registry study finds no increased risk of cancer recurrence with bDMARDs vs csDMARDs in RA patients with prior solid tumor in remission. IPTW-adjusted HR for any bDMARD: 0.92 (95% CI 0.38–2.21).
📉 TNFi, ,RTX also not associated with recurrence
@RheumNow #EULAR2025
Jiha Lee JihaRheum ( View Tweet)

In #InflammatoryArthritis, baseline depression was linked to ↑ presenteeism & ↓ QoL at baseline + 3mo, but not absenteeism. Data from 9-country study provide further evidence that mental health is key to supporting work outcomes in RA, PsA & axSpA.
@RheumNow #EULAR2025 #OP0028
Mrinalini Dey DrMiniDey ( View Tweet)

Worried about cancer risk with ts/bDMARDs in RA?
Real-world data from over 4,600 patients says: don’t be. No increased risk of cancer (incl. NMSC) for JAKi, IL6i, CD20i, or CTLA4-A vs TNFi in long-term registry follow-up.
Abstract#OP0065
@RheumNow #EULAR2025
Jiha Lee JihaRheum ( View Tweet)

STAMP RCT early SEC vs. SoC 120pts
Retention 58% vs 30%
ACR 20, 50, 70 and MDA: better outcome at Month 3 but no difference at Month 6
Dactylitis no difference
Of note here SoC was a tight T2T strategy!
@RheumNow #OP0092 #EULAR2025 https://t.co/8zHs5CRFV5
Links:
Aurelie Najm AurelieRheumo ( View Tweet)
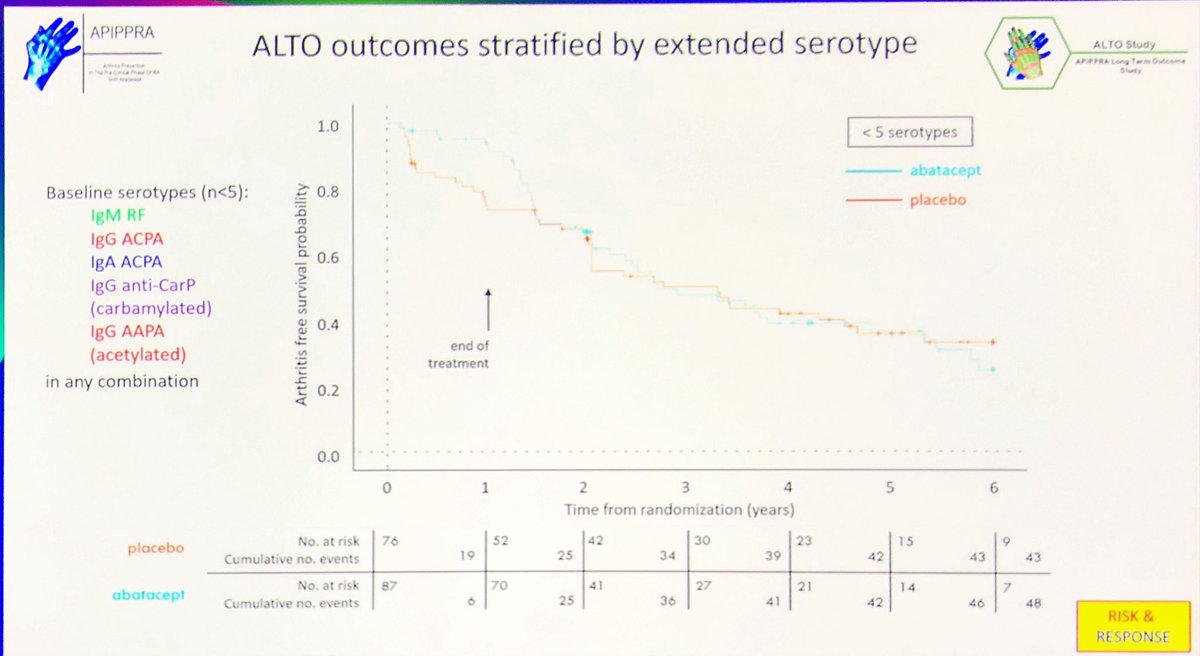
What happens in pre-RA when you stop #abatacept after 1 yr Rx
At 6 yrs approx 60% on #Placebo
V
50% who initially got #ABA
Prolonged damped effect of development of #RA
NNT for 1 yr is ~10 with a range as low as 6
#EULAR2025 @RheumNow @eular_org
Abst#OP0004 https://t.co/1VOEaZ00Ia
Links:
Janet Pope Janetbirdope ( View Tweet)
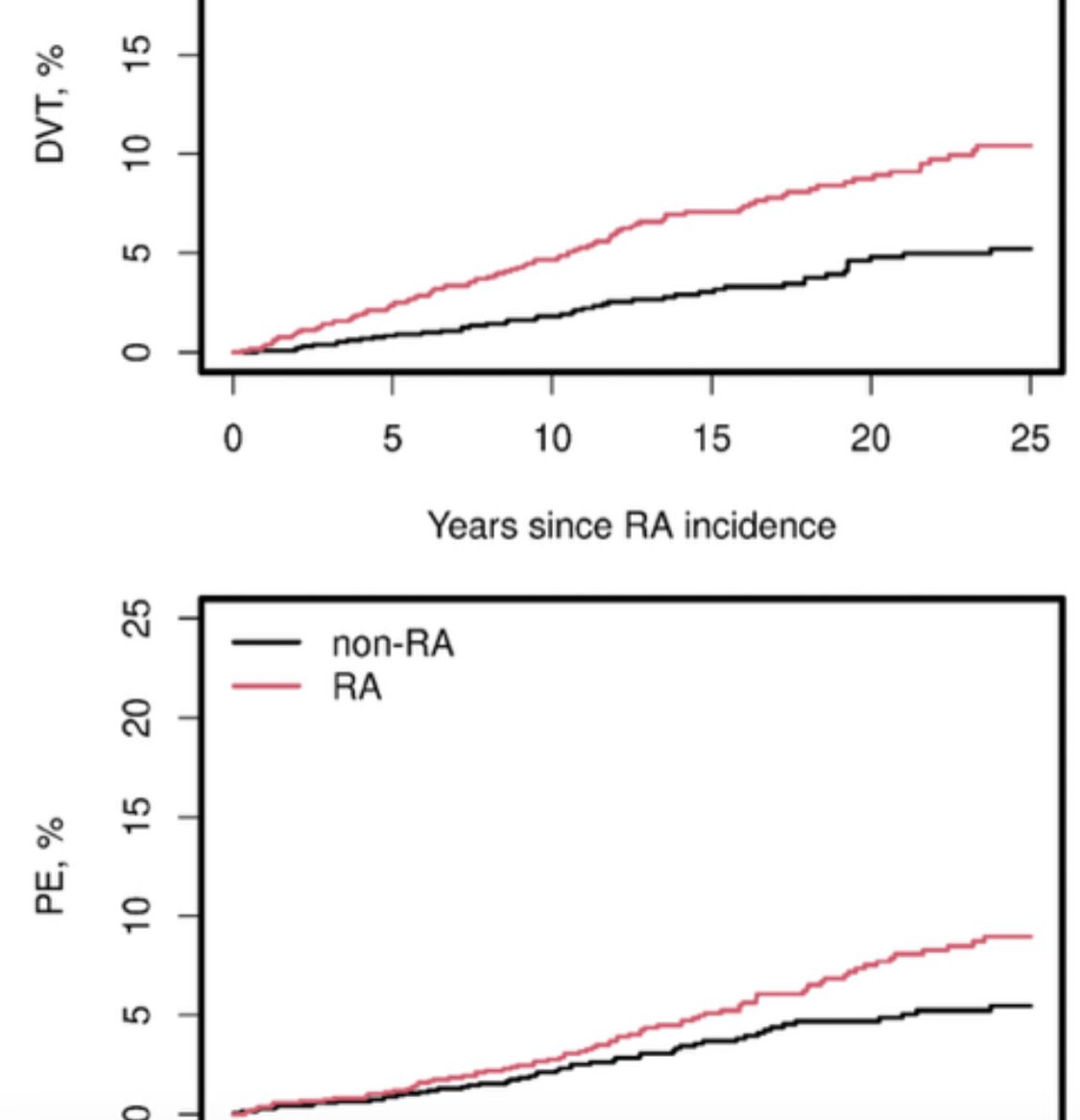
Risk of #VTE in #rheumatoid #arthritis
Is it better over last 25 yrs?
👎
Olmstead
County population study of #RA Pts vs matched controls
⬆️VTE in RA
⬆️VTE w active RA
But not change in rates of #DVT & #PE since 2000
Why? 🤔
Abst#OP0070 @rheumnow #EULAR2025 @eular_org https://t.co/eSyjfjVqtY
Janet Pope Janetbirdope ( View Tweet)
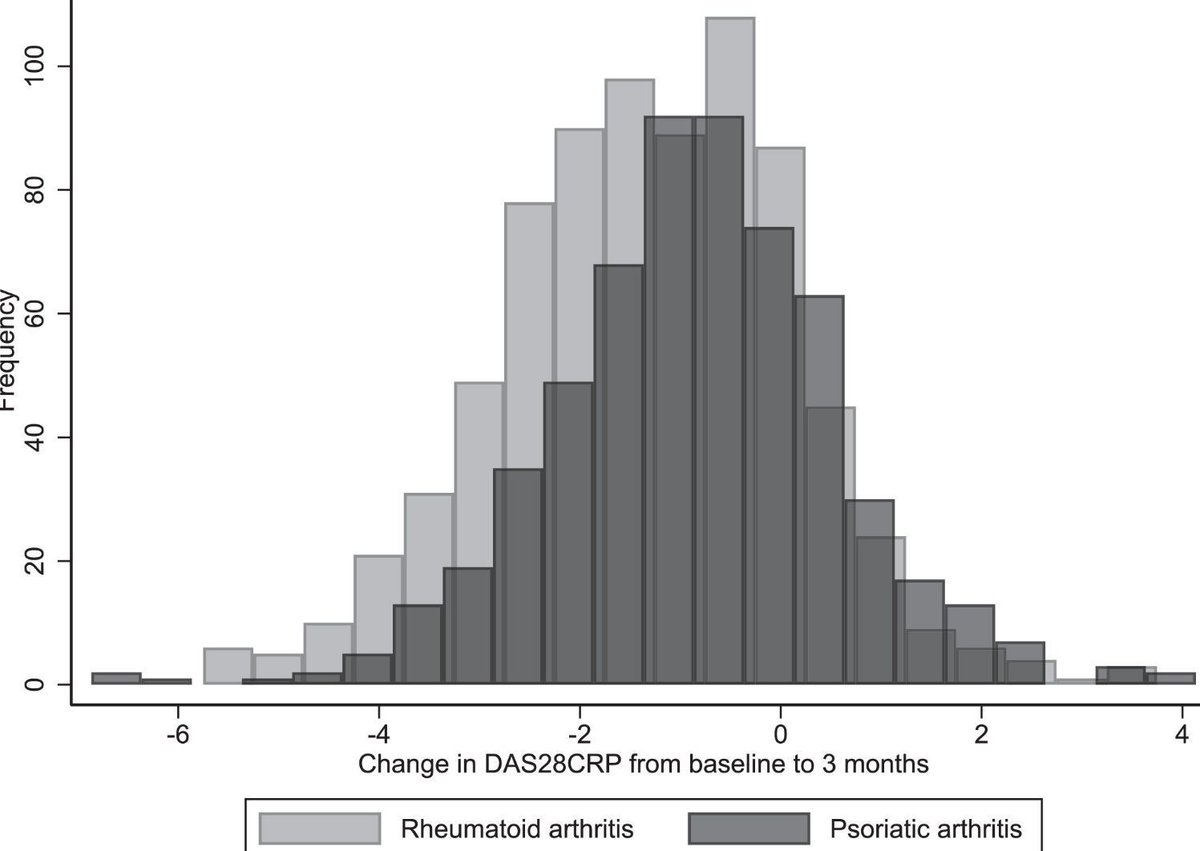
UK Natl Early Inflammatory Arthritis Audit (5/18-11/19) compared 2120 PsA & RA (1:1). PsA had longer Sx to referral wait (112 v 89 days; HR 0.87), longer delay in Dx (HR 0.8), PsA less DMARD use at baseline (54% v 69%) & higher DAS28 results at 3 mos (+0.27) https://t.co/zyubhGxw47
Dr. John Cush RheumNow ( View Tweet)
POSTER HALL PRESENTATION: Sponsored by AbbVie Medical Affairs + Health Impact.
🔍Real-world outcomes in patients with RA remaining on first-line TNFi
📽️See Dr. Charles-Schoeman discuss subsequent outcomes in patients who did or did not achieve response at 3 or 6 months https://t.co/8RmcigG7SF
Dr. John Cush RheumNow ( View Tweet)

Otilimab, GM-CSF mAb, may have potential in #RA. Metanalysis of 4 RCTs, w/ 3933 RA pts had Moderate evidence for ACR20 response (vs PBO) at 90 mg (RR 1.50) & 150 mg (RR 1.39). but neither dose had signif different adverse events vs PBO. OTIL was less effective than tofacitinib. https://t.co/2WajWNnxE9
Dr. John Cush RheumNow ( View Tweet)
Positive results from Phase 2b RENOIR RCT of Rosnilimab, an agonist targeting PD-1+ T cells. 432 RA pts on MTX or csDMARDs, Rx w/ 6 mos of PBO vs ROS (100 or 200 mg q4wk or 600 mg q2wk). All 3 doses of rosnilimab achieved significant reductions DAS-28 CRP at Wk 12 https://t.co/g7lqQYXeJd
Dr. John Cush RheumNow ( View Tweet)

Extract of purple sweet potato ANTHOCYANINS (PSPA) studied in CIA animal model of #RA; Rats Rx w PBO or PSPA (10, 20, or 40 mg/kg) x14days. 40mg/kg dose reduced synovitis, altered gut microbiota (Akkermansia, Lactobacillus) decr RF & cytokines TNF-α, IL-1β, IL-6, IL-18) https://t.co/UjPFEuTU1S
Dr. John Cush RheumNow ( View Tweet)

Swiss Registry study of PsA outcomes when started on either TNFi (N 503) or IL-17i (n 341), latter w/ more severe PSO. IL-17i durability superior to TNFi (median 828 vs 445 d, P<.001), w/ less D/C in women (HR 0.57); but ACR 20 (14 v 33%) & ACR50 (7 v 24%) favored TNFi use https://t.co/R33bwSeB3E
Dr. John Cush RheumNow ( View Tweet)

Positive results from Phase 2b RENOIR RCT of Rosnilimab, an agonist targeting PD-1+ T cells. 432 RA pts on MTX or csDMARDs, Rx w/ 6 mos of PBO vs ROS (100 or 200 mg q4wk or 600 mg q2wk). All 3 doses of rosnilimab achieved significant reductions DAS-28 CRP at Wk 12 https://t.co/6nF8KPRK2f
Dr. John Cush RheumNow ( View Tweet)
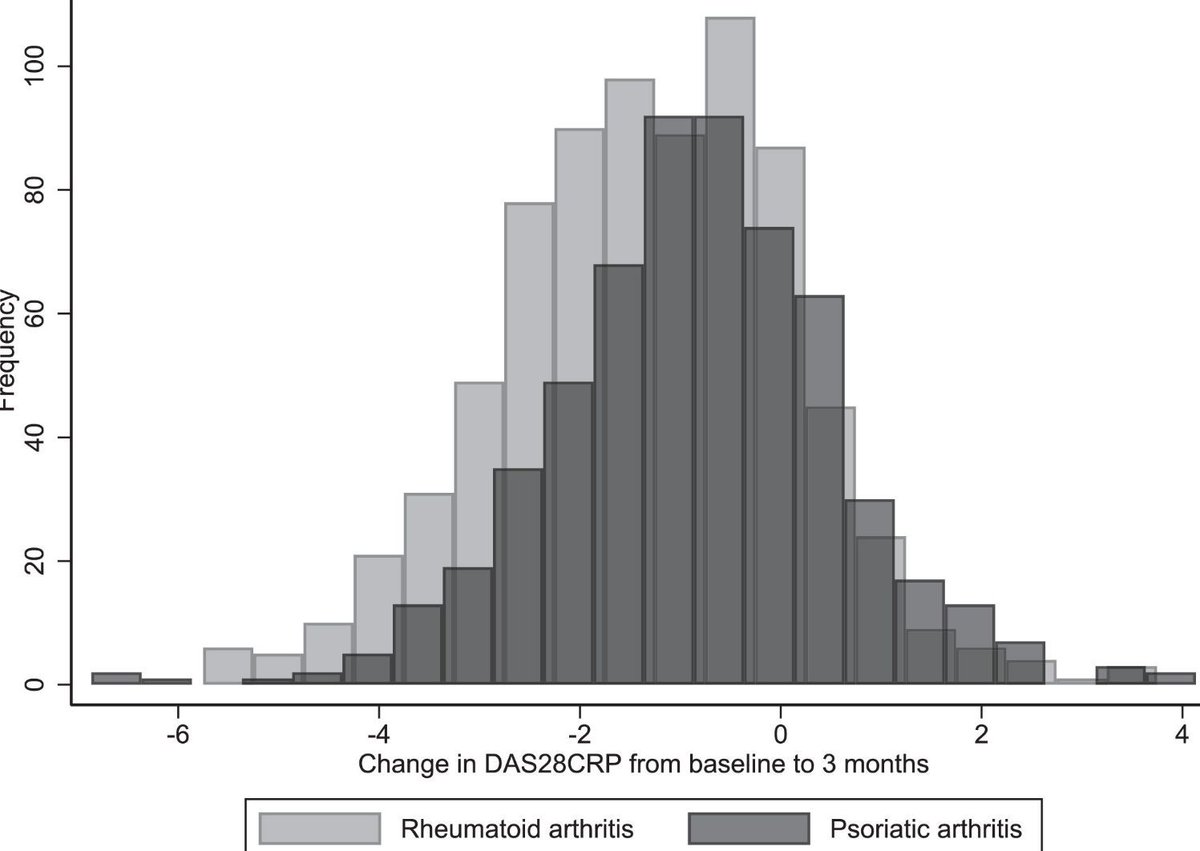
UK Natl Early Inflammatory Arthritis Audit (5/18-11/19) compared 2120 PsA & RA (1:1). PsA had longer Sx to referral wait (112 v 89 days; HR 0.87), longer delay in Dx (HR 0.8), PsA less DMARD use at baseline (54% v 69%) & higher DAS28 results at 3 mos (+0.27) https://t.co/ObssKGcomq
Dr. John Cush RheumNow ( View Tweet)





