All News
Stress Raises the Risk of Psoriasis
New longitudinal research reveals that severe stress caused by changes in family structure like divorce or separation experienced during the first year of life may triple the risk of developing psoriasis later in life.
Read ArticleCan Steroids Be Stopped in Lupus Nephritis?
Patients with lupus nephritis were more likely to get off chronic corticosteroid treatment, and stay off, when certain factors were in place, researchers said.
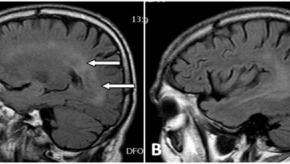
Read ArticleClinical and Genetic Effects of Neuropsychiatric Lupus
The clinical features and genetic abnormalities of neuropsychiatric systemic lupus erythematosus shows that NPSLE often means more severe lupus and more organ involvement beyond the central nervous system.
Read ArticleREPLENISH - Secukinumab Works in Polymyalgia Rheumatica
Novartis announced the results of their REPLENISH trial showing the efficacy of secukinumab in adults with polymyalgia rheumatica (PMR).
Read ArticleColchicine Ineffective in Long COVID
Management of long COVID has been perplexing with symptoms having functional and possibly inflammatory origins. Colchicine has been studied in long COVID and failed to improve functional capacity, respiratory function, or inflammatory markers.
Read Article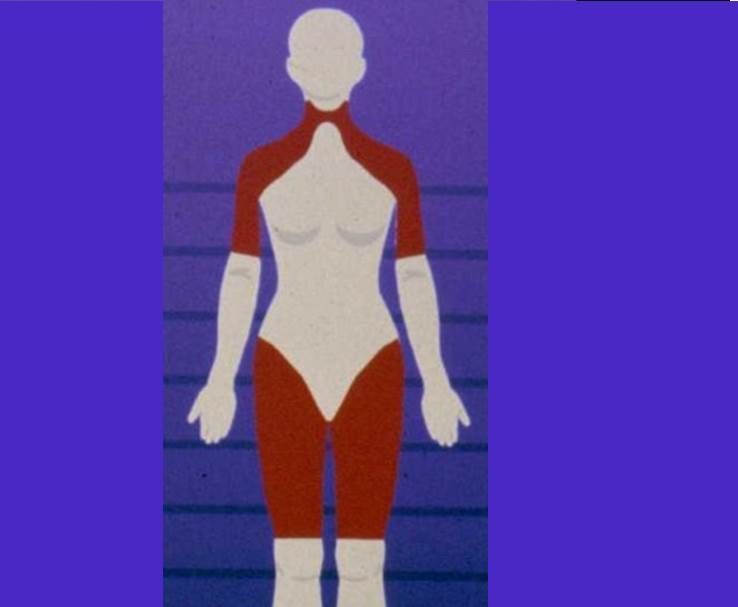
Links: