Clinical and Genetic Effects of Neuropsychiatric Lupus Save
The clinical features and genetic abnormalities of neuropsychiatric systemic lupus erythematosus shows that NPSLE often means more severe lupus and more organ involvement beyond the central nervous system.
NPSLE may affect at many as half of all SLE patients, and is a severe complication of SLE, that is often difficult to diagnose and manage. This study aimed to identify the clinical features of NPSLE and explore genetic factors associated with NPSLE in a prospective lupus cohort.
From a large lupus cohort of 1205 Korean patients (seen at least annually), 271 (22.5%) had NPSLE.
Importantly, NPSLE patients had significantly more clinically diverse manifestations (p=2.40×10−4), especially in patients with seizure (N=84, p=4.86×10−14) and psychosis (N=26, p=8.29×10−5), compared to 934 patients without NPSLE.
NPSLE patients significantly had greater organ damage (by SLICC score; OR 1.49, p=3.28×10−17;) after adjusting for age, sex, hypertension, disease duration and antiphospholipid antibodies.
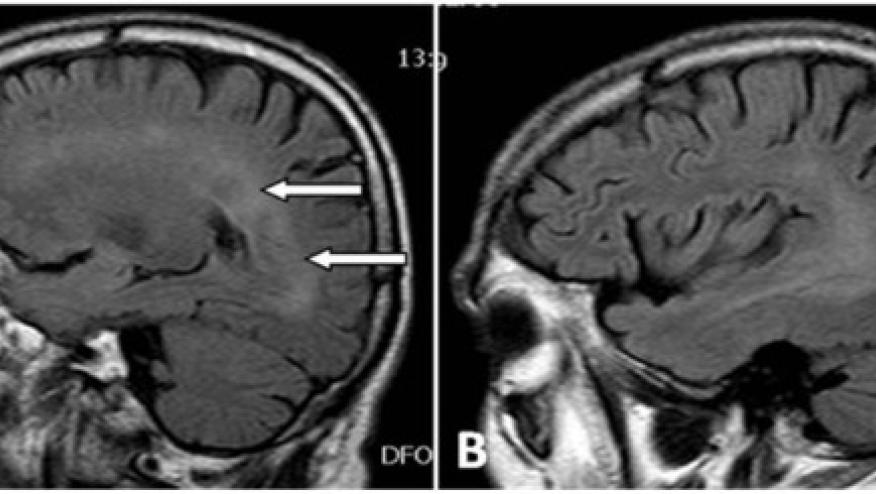
GWAS revealed nine NPSLE-associated loci at a suggestive significance level (p<5×10⁻⁶). The nine nearest mapped genes were exclusively expressed in the brain (adjusted p=5.28×10−4), particularly in the basal ganglia, cortex and hippocampus (adjusted p<0.05).
Neuropsychiatric involvement in SLE significantly complicates lupus manifestations beyond the nervous system. NPSLE-related genes are significantly enriched in the brain, particularly the basal ganglia, cortex and hippocampus, thusly enhancing our understanding of the genetic basis and neurobiological mechanisms underlying NPSLE.










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.