Antifibrotics - A New Class of Therapies in Rheumatology? Save
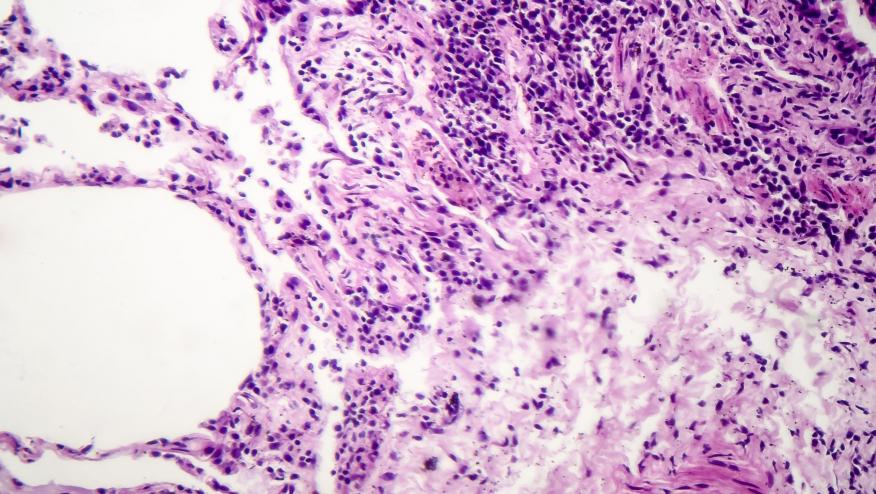
Rheumatologists typically manage systemic autoimmune rheumatic diseases (SARD) and associated interstitial lung disease (ILD) with immunosuppressants. However, evidence increasingly supports also the use of antifibrotic agents in this setting. Pulmonologists have long used antifibrotics for ILD caused by idiopathic pulmonary fibrosis (IPF) and other conditions, but rheumatologists have limited experience with these drugs. Although patients with IPF generally have a worse prognosis than those with SARD-ILD, epidemiologic data show that patients with progressive pulmonary fibrosis in SARD-ILD—particularly those with a ≥10% decline in forced vital capacity (FVC%) over the past year—have outcomes similar to IPF. This underscores the urgent need to expand treatment options in this area.
To address this unmet clinical need, the randomized, double-blind INBUILD trial tested the antifibrotic agent, nintedanib, in progressive ILDs other than IPF and showed a significant reduction in annual FVC decline¹. As a basket trial, INBUILD included patients with diverse ILDs (25% had SARD-ILD), based on the hypothesis that fibrosing ILDs, despite different triggers, share a final common fibrotic pathway targetable by antifibrotics. The SENSCIS trial further evaluated nintedanib in systemic sclerosis (SSc)-ILD2. Unlike INBUILD, it did not require disease progression and allowed background mycophenolate treatment. Of 570 enrolled patients, about half were on mycophenolate. Nintedanib significantly slowed FVC decline compared with placebo. Diarrhea was the most frequent side effect, affecting 76% of treated patients versus 32% on placebo. Based on these data, the FDA approved nintedanib for SSc-ILD and progressive fibrosing ILD.
Pirfenidone, another antifibrotic approved for IPF, was studied in rheumatoid arthritis (RA)-ILD in the TRAIL1 trial3. The primary endpoint was the incidence of the composite endpoint of a decline from baseline in FVC% of 10% or more or death. Although this study was stopped early due to slow recruitment and the COVID-19 pandemic, 183 patients were randomized to pirfenidone or placebo. There was no significant difference in the composite primary endpoint, but patients in the pirfenidone group had a significantly slower rate of decline in FVC compared to the placebo group. There are no other large-scale studies examining the efficacy of pirfenidone in SARD-ILDs. Moreover, pirfenidone is only FDA-approved for the treatment of IPF, restricting its use in SARD-ILDs.
While the above studies indicate that antifibrotic agents are effective in treating SARD-ILDs, their utilization in rheumatology remains limited. This is in part due to the high rate of gastrointestinal side effects of nintedanib, but also due to the unfamiliarity of the rheumatology community with this class of medications and the management of their side effects. The recently completed FIBRONEER-ILD examined the efficacy of nerandomilast (a preferential phosphodiesterase 4B [PDE-4b] inhibitor) for the treatment of progressive fibrosing ILD4. Similar to the INBUILD trial, this study was a basket trial that included 1176 progressive fibrosing ILD patients caused by different diseases (25% of whom had SARD-ILD). Nerandomilast significantly slowed the rate of decline in FVC compared to placebo over 52 weeks. Notably, nerandomilast also showed a survival benefit compared to placebo. While background treatment with nintedanib was permitted, patients who were on mycophenolate at the baseline visit were excluded. This is a limitation of the present study that can be addressed in future studies. In terms of side effects, the rate of diarrhea in the nerandomilast monotherapy group in the FIRBONEER-ILD trial was substantially lower than the rate of this side effect in the nintedanib-treated group in the INBUILD-Trial, suggesting that this medication might have a better gastrointestinal side-effect profile than nintedanib. Moreover, there were no imbalances regarding adverse events of interest observed with other PDE-4 inhibitors, such as depression or suicidality, between the nerandomilast and placebo groups. These findings suggest nerandomilast may offer a better-tolerated antifibrotic option for SARD-ILD.
In summary, recent large-scale clinical trials have broadened therapeutic options for SARD-ILD beyond immunosuppressants, offering new hope for patients with these serious conditions.
1. Flaherty KR, Wells AU, Cottin V, Devaraj A, Walsh SLF, Inoue Y, Richeldi L, Kolb M, Tetzlaff K, Stowasser S, Coeck C, Clerisme-Beaty E, Rosenstock B, Quaresma M, Haeufel T, Goeldner RG, Schlenker-Herceg R, Brown KK; INBUILD Trial Investigators.Nintedanib in Progressive Fibrosing Interstitial Lung Diseases N Engl J Med. 2019 Oct 31;381(18):1718-1727.
2. Distler O, Highland KB, Gahlemann M, Azuma A, Fischer A, Mayes MD, Raghu G, Sauter W, Girard M, Alves M, Clerisme-Beaty E, Stowasser S, Tetzlaff K, Kuwana M, Maher TM; SENSCIS Trial Investigators. Nintedanib for Systemic Sclerosis-Associated Interstitial Lung Disease. N Engl J Med. 2019 Jun 27;380(26):2518-2528.
3. Solomon JJ, Danoff SK, Woodhead FA, Hurwitz S, Maurer R, Glaspole I, Dellaripa PF, Gooptu B, Vassallo R, Cox PG, Flaherty KR, Adamali HI, Gibbons MA, Troy L, Forrest IA, Lasky JA, Spencer LG, Golden J, Scholand MB, Chaudhuri N, Perrella MA, Lynch DA, Chambers DC, Kolb M, Spino C, Raghu G, Goldberg HJ, Rosas IO; TRAIL1 Network Investigators.Safety, tolerability, and efficacy of pirfenidone in patients with rheumatoid arthritis-associated interstitial lung disease: a randomised, double-blind, placebo-controlled, phase 2 study. Lancet Respir Med. 2023 Jan;11(1):87-96.
4. Maher TM, Assassi S, Azuma A, Cottin V, Hoffmann-Vold AM, Kreuter M, Oldham JM, Richeldi L, Valenzuela C, Wijsenbeek MS, Clerisme-Beaty E, Coeck C, Gu H, Ritter I, Schlosser A, Stowasser S, Voss F, Weimann G, Zoz DF, Martinez FJ; FIBRONEER-ILD Trial Investigators.Nerandomilast in Patients with Progressive Pulmonary Fibrosis. N Engl J Med. 2025 Jun 12;392(22):2203-2214.
Dr. Assassi reports grant funding from Janssen, Abbvie, and Boehringer Ingelheim to his Institution and personal consultancy/speaking fees from Abbvie, AstraZeneca, aTyr, Boehringer Ingelheim, CSL Behring, Merck, Mitsubishi, Regeneron, Takeda
Join The Discussion
excellent short review.










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.