5 Fractures You Don’t Want to Miss Save

In orthopedic practice, missing the wrong fracture can significantly alter a patient’s outcome. Certain injuries may appear subtle on initial imaging yet carry serious consequences if not promptly recognized and managed. Below are five fractures that warrant a high index of suspicion due to their risk of displacement, nonunion, or long‑term degenerative change.
Femoral Neck Fractures
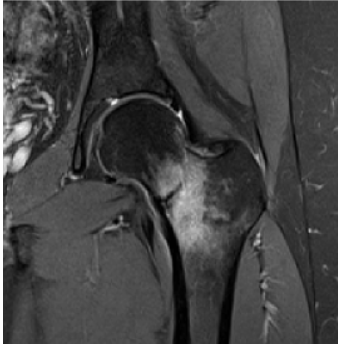
Femoral neck fractures are commonly seen in elderly patients after low‑energy falls, as well as in younger patients following high‑energy trauma such as motor vehicle accidents. While many are readily apparent on hip or pelvis radiographs, femoral neck stress fractures can be more elusive. These injuries occur from repetitive loading, often in runners or military personnel. If missed, continued weightbearing can lead to fracture displacement or femoral head avascular necrosis. In patients with persistent groin or thigh pain and negative radiographs, MRI is indicated. Early diagnosis allows for protected weightbearing and prevents progression to catastrophic injury.
Jones Fractures
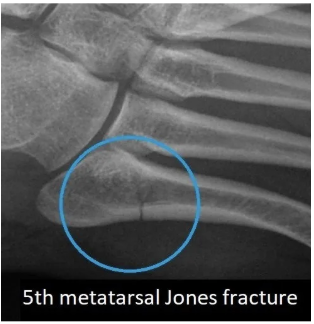
A Jones fracture involves the fifth metatarsal at the metaphyseal‑diaphyseal junction, an area with a known vascular watershed. This compromised blood supply increases the risk of delayed union and nonunion. Patients typically present with lateral foot pain, swelling, and ecchymosis following a twisting or inversion injury. While diagnosed on standard foot radiographs, failure to correctly identify the fracture zone may result in inappropriate weightbearing recommendations. Patients should be placed non‑weightbearing in a short leg splint and referred to orthopedics.
Scaphoid Fractures

Scaphoid fractures are another injury prone to nonunion due to retrograde blood supply, particularly at the waist of the bone. Missed fractures can progress to scaphoid nonunion advanced collapse (SNAC) and post‑traumatic wrist arthritis. Patients often present with anatomic snuffbox tenderness following a fall onto an outstretched hand. Although fractures may be visible on standard three‑view wrist radiographs, MRI is warranted when clinical suspicion remains high despite negative x‑rays. Immobilization in a thumb spica splint and referral to a hand specialist are essential.
Maisonneuve Fractures

A Maisonneuve fracture represents a complex ankle injury involving syndesmotic and deltoid ligament disruption with an associated proximal fibular fracture, typically caused by an external rotation mechanism. Patients may have ankle pain, medial tenderness, proximal fibular pain, and difficulty weightbearing. Diagnosis requires careful evaluation with ankle radiographs for medial clear space widening and tibia/fibula imaging to assess the proximal fibula. These injuries are frequently misdiagnosed as isolated ankle sprains, leading to chronic instability and post‑traumatic ankle arthritis if untreated.
Lisfranc Fractures-Dislocations

Lisfranc injuries involve disruption of the tarsometatarsal articulation between the second metatarsal base and medial cuneiform, stabilized by the Lisfranc ligament. While severe injuries may be obvious on initial imaging, subtle cases may only demonstrate widening between the first and second metatarsals or a small avulsion “fleck sign.” Missed Lisfranc injuries predictably result in painful post‑traumatic midfoot arthritis. When radiographs are inconclusive, MRI is helpful to evaluate for ligamentous injury and occult fractures. Prompt non‑weightbearing immobilization and orthopedic referral are critical.
Bottom line: These fractures may be infrequent, subtle, or easily misdiagnosed, but early recognition and appropriate management can prevent long‑term morbidity. Maintaining a high index of suspicion—and knowing when to pursue advanced imaging—can make all the difference.
Visit our Mission APP: Partners in Care site for more APP-focused articles and videos.










If you are a health practitioner, you may Login/Register to comment.
Due to the nature of these comment forums, only health practitioners are allowed to comment at this time.